Background: Ischemic heart disease (IHD) and chronic obstructive pulmonary disease (COPD) are significant causes of morbidity and mortality globally. Understanding temporal trends in mortality related to IHD among COPD patients in U.S. population is crucial for guiding clinical practice and public health interventions.
Methods: Death certificates from the CDC WONDER (Centers for Disease Control and Prevention Wide-Ranging Online Data for Epidemiologic Research) database were analyzed spanning from 1999 to 2020 to investigate mortality related to ischemic heart disease (IHD) in individuals aged over 35 years with chronic obstructive pulmonary disease (COPD). Age Adjusted mortality rates (AAMRs) per 100,000 persons and annual percent change (APC) were computed, and the data were stratified by year, sex, race/ethnicity, and geographic region.
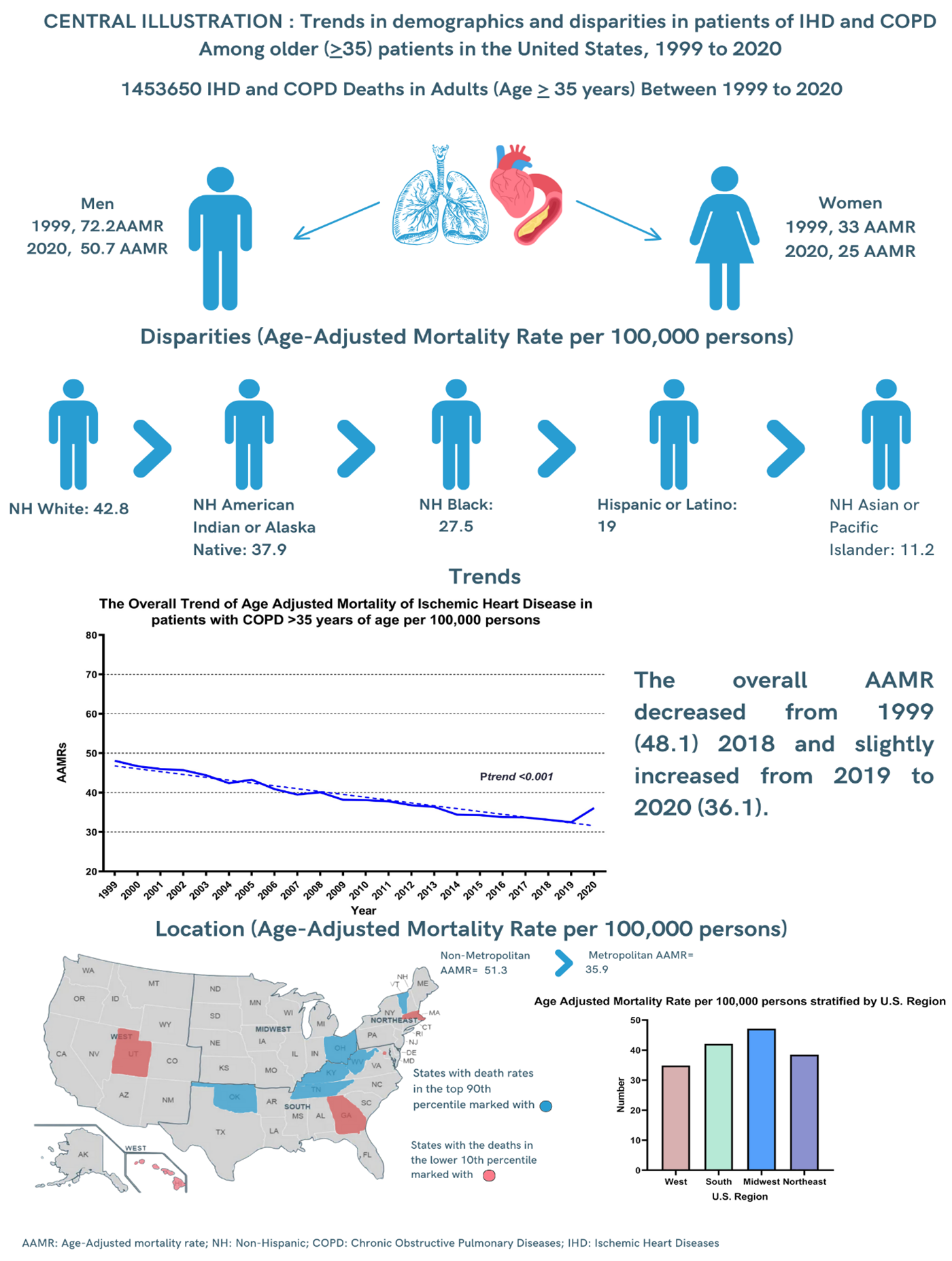
Results: A total of 1,453,650 deaths occurred among adults (aged 35-85 + years) between 1999 and 2020 related to IHD in COPD patients. The overall AAMR decreased from 1999 to 2018 (APC: -2.02; 95% CI: -2.19 to -1.83) followed by an Increase from 2018 to 2020 (APC: 4.51; 95% CI: 1.34-6.02). Men had consistently higher AAMRs than adult women throughout the study period (overall AAMR men: 55, 95% CI: 54.9-55.1; women: 27.1, 95% CI: 27.1-27.2). The AAMR for adult men and women at the end of the study period was 50.7 and 25.1, respectively (Men: 95% Cl: 50.2-51.2; women: 95% CI: 24.8-25.4). White adults had the highest overall AAMR (42.8), followed by NH American Indian/Alaska Native (37.9), NH Black or African American (27.5), Hispanic or Latino (19), and NH Asian or Pacific Islander adults (11.2). States that fell into the top 90th percentile were West Virginia, Vermont, Tennessee, Ohio, Oklahoma, and Kentucky, which had approximately three times the AAMRs compared with states that fell into the lower 10th percentile, namely, Hawaii, Georgia, District of Columbia, Massachusetts, and Utah. AAMR also varied by region (overall AAMR: Midwestern: 43.1; South: 40.3; Western: 34.8; Northeast: 34.4), and nonmetropolitan areas had higher IHD and COPD-related AAMR (51.3) than metropolitan areas (35.9).
Conclusions: Temporal trends in mortality related to IHD among COPD patients showed fluctuations over the study period, with notable disparities across demographic and geographic factors. These findings underscore the need for targeted interventions to address the burden of IHD among COPD patients and reduce mortality rates in the United States.