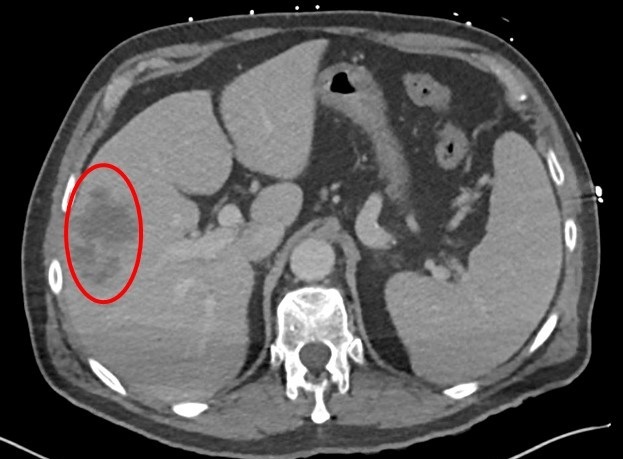
Case Presentation: Patient was a 57-year-old female with medical history of type II diabetes mellitus who presented with intermittent fevers, chills and abdominal pain. Labs were unremarkable except for mild transaminitis. Imaging revealed a right hepatic lobe lesion and moderate right pleural effusion. Blood cultures grew Strep intermedius in ¼ bottles, but repeat cultures were negative. A diagnostic thoracentesis was performed, but cytology and fluid cultures were negative. Liver biopsy was consistent with a pyogenic abscess; tissue cultures grew MRSA. She was discharged on Linezolid.She was readmitted two weeks later with a large right pleural effusion. A chest tube was inserted, draining serosanguineous fluid. It was later removed but repeat imaging revealed re-accumulation of pleural effusion and a right-lobe hepatic abscess. As a result, a second chest tube and a JP drain were placed into the hepatic abscess. Due to insufficient drainage, the patient underwent tPA instillation into the pleural cavity. This was complicated by hemothorax necessitating an emergent VATS with decortication, which showed a hepatic-pleural fistula, with JP drain traversing the diaphragm and resting in the pleural space. The drain was removed while the chest tube was left in place. Pleural fluid cultures and cytology remained sterile. Her symptoms resolved completely after the procedure, and the chest tube was removed after repeated negative chest imaging. She was discharged on oral linezolid and outpatient follow-up with Infectious Disease and Pulmonology.
Discussion: Pyogenic hepatic abscess is an uncommon but potentially life-threatening condition. Most cases arise from biliary sources, namely stricture, malignancy, choledocholithiasis and cholangitis. Less common causes include trauma, hematogenous spread from other organs, and appendicitis, to name a few. It is not uncommon to develop a pyogenic hepatic abscess without an identifiable infectious source. As most cases arise from intra-abdominal sources, they are usually polymicrobial with anaerobic and gram-negative prominence.Our case was diagnostically challenging as the blood cultures grew Streptococcus intermedius, a bacterium commonly implicated in liver abscesses and fistulas. However, the abscess cultures grew MRSA. We believe that Streptococcus intermedius served as a vector for MRSA.MRSA is an uncommon cause of pyogenic abscesses, especially in the absence of positive blood cultures. It has been mostly described in elderly, immunocompromised, incarcerated populations or those who recently had abdominal procedures. Our patient did not have any of these risk factors. A transthoracic echocardiogram was obtained to rule out infective endocarditis, and it did not show any vegetation. Treatment of a hepatic abscess involves drainage and culture-directed antimicrobial treatment. Hepatic abscess can cause right-sided pleural effusion due to diaphragmatic and pleural irritation. However, the formation of a hepato-pleural fistula and empyema is an infrequent finding, especially in immunocompetent patients. In such cases, drainage of the empyema with a chest tube remains the mainstay of the treatment followed by lytic therapy if needed. VATS can also be used if all other treatments fail. Culture-directed antimicrobials usually follow this until resolution.
Conclusions: MRSA is an uncommon cause of pyogenic hepatic abscess in immunocompetent patients. In rare instances, it can lead to the formation of trans-diaphragmatic tract and empyema.