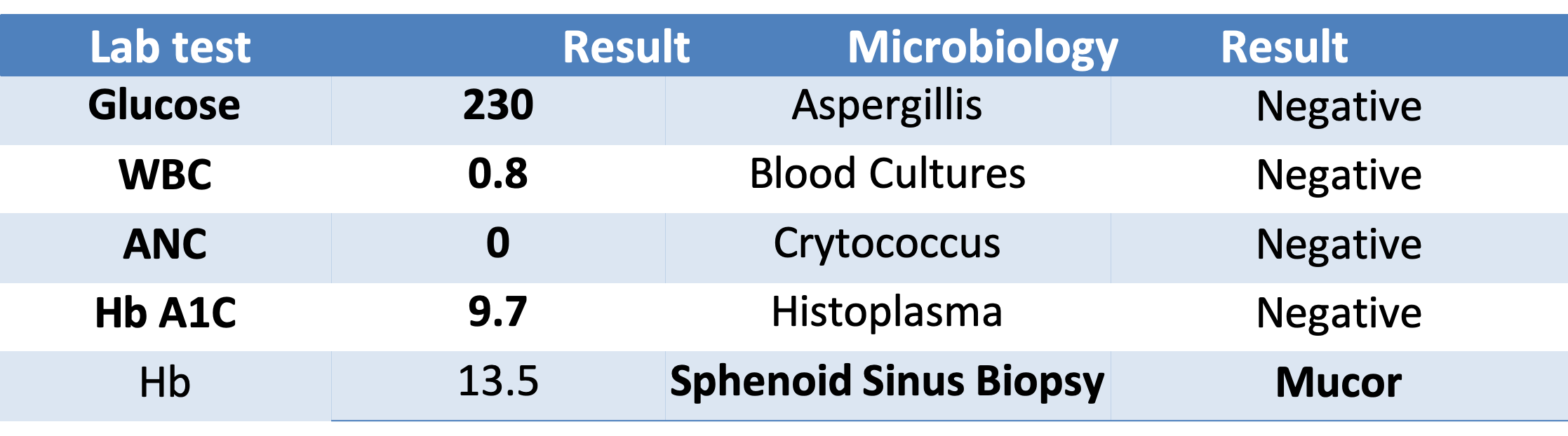
Case Presentation: A 54 year-old Hispanic man with a history of deep vein thrombosis (DVT) and glioblastoma multiforme treated with right parietal craniotomy and temozolomide, presented with fever, headache, and odynophagia. He reported a week of odynophagia with solids and liquids, worsening headaches, and fever of 100.4 F. His last cycle of temozolomide and radiation was one month prior, and he recently discontinued rivaroxaban for treatment of DVT due to bleeding. His only medication was dexamethasone. Vitals were unremarkable. Physical exam was notable for a white plaque in his oropharynx and left-sided weakness stable from his prior craniotomy. Labs demonstrated an absolute neutrophil count (ANC) of 0, and glucose of 230. He was started on cefepime for neutropenic fever. No infectious source was identified through cultures or imaging.Three days later, the patient developed sudden-onset diplopia and cranial nerve (CN) VI palsy. Emergent imaging was ordered due to concern for stroke. His CT head showed no hemorrhage and his MRI showed no evidence of acute infarct or tumor changes. CN VI palsy was considered to be a false localizing sign due to increased intracranial pressure (ICP) from his tumor and dexamethasone was increased. However, no papilledema was noted to support increased ICP.Closer review of his MRI revealed new air-fluid levels in the ethmoid sinus. Given his constellation of symptoms including headache, fever, severe neutropenia, hyperglycemia, and now ocular involvement, Amphotericin B was empirically started along with surgical consultation. Given high suspicion for invasive fungal infection, he was rushed to Operating Room for debridement. The surgical pathology returned positive for mucor. His eyes and nose were salvaged after three operations. He was discharged on a prolonged course of oral posaconazole.
Discussion: Given the broad differential of neurologic etiologies for his symptoms (hypercoagulability, brain tumor, febrile neutropenia), diagnosis in this patient was challenging. The only way to definitely diagnose mucormycosis is through biopsy. The primary pillar of treating mucor is emergent surgical debridement and amphotericin, though tight glucose control, immune reconstitution, and correction of acidosis also improve survival. Newer adjunctive treatment modalities such as hyperbaric oxygen, iron chelators, and immune therapy are on the horizon for treating this lethal disease. Keeping a high index of clinical suspicion to detect mucormycosis is the key for prompt diagnosis and better outcomes.
Conclusions: Consider mucor on your differential for patients with fever, headache, and cranial nerve palsies especially if immunocompromised. Identify prompt initiation of Amphotericin and surgical debridement as the treatment of rhinocerebral mucormycosis.