Background: Successful hospitalist co-management programs address provider knowledge base as well as ongoing faculty skill development and education (1). With a growing liver transplant program, our institution has seen increased patient volume on the hospitalist liver service. Hospitalists and hepatologists co-manage this expanding population of high acuity patients with complex pathologies. In the past year, we have added a liver overflow team and 27 hospitalists to the section. These new hires had varied past experiences and exposure to liver and liver transplant patients.
Purpose: We aimed to develop a curriculum for liver co-management to optimize patient care via the improvement of provider satisfaction and strengthening of multi-specialty teamwork and education between Hospital Medicine (HM) physicians and Advanced Practice Providers, Hepatology, and Transplant Pharmacy.
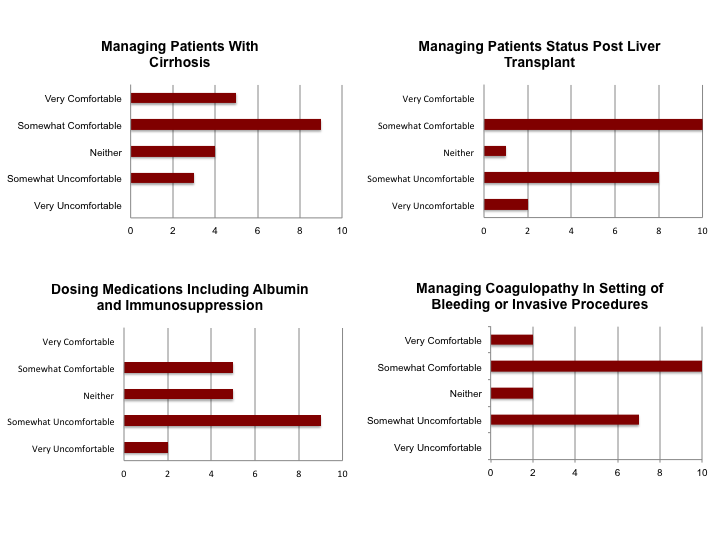
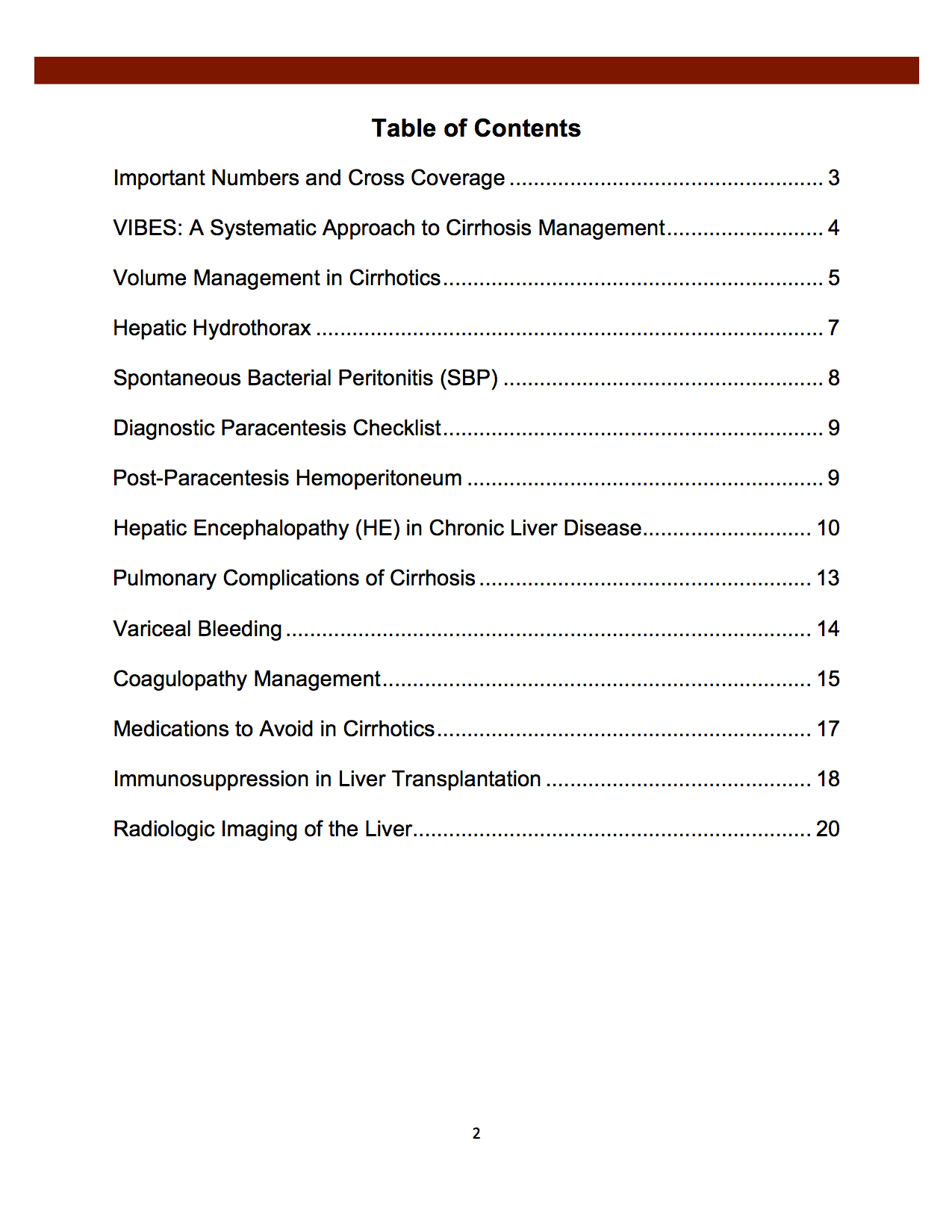
Description: An initial needs assessment was created to gauge hospitalist confidence in hepatology clinical knowledge. Completed by 21 of our new hospitalists, this data showed overall lack of comfort with management of liver patients, especially transplant recipients and medication dosing (figure 1). Facilitated by a HM transplant liaison, we conducted multidisciplinary focus groups to identify the greatest areas of need for our co-management model. We noted a deficiency of available reference material to guide standardized care of common liver diagnoses. Learning objectives were developed to address high-yield topics (figure 2), including evidence-based and site-specific management strategies. The HM Liver and Liver Transplant Manual was written and edited in collaboration with involved specialties. A smart phone compatible format for quick reference was distributed electronically. Education and service updates were disseminated through live onboarding sessions for new hospitalists, emails, meetings, and CME lectures from hepatologists on topics with a HM focus. Our novel co-management curriculum will be evaluated with longitudinal surveys, quantifying use of the manual and trending provider engagement metrics like satisfaction and team recruitment. Based on the manual, we are developing resources to further standardize and streamline workflow with EMR based clinical pathways and order sets, also with a multi-specialty based approach.
Conclusions: While improved quality of care is recognized in hospitalist-led liver co-management models (2), the ideal method to establish and maintain provider proficiency and adherence to evidence-based guidelines through education and resources is uncertain. Co-management HM and medical sub-specialty teams have the distinctive ability to increase specialist and hospitalist provider engagement while creating multi-specialty developed curriculum.