Case Presentation: A 21-year-old Hispanic male with no past medical history presented to our hospital with worsening abdominal pain for approximately two months. He described the pain as initially intermittent but progressive and was not associated with eating food. In addition, he also complained of a diffuse maculo-papular rash involving the palms and soles that persisted despite treatment with over the counter topical creams along with swelling of his lower extremities. Remainder of review of systems were negative. On presentation, he was afebrile with normal vital signs. He had a enlarged submandibular and right inguinal nodes with crackles on lower right lung fields, with some mild abdominal tenderness to palpation. A maculopapular rash on his soles and palms was noticed. His laboratory tests were significant for positive HIV, with CD 4 of 175 and viral load of 217000 cpy/ml, with positive RPR. Remainder of labs were unremarkable.
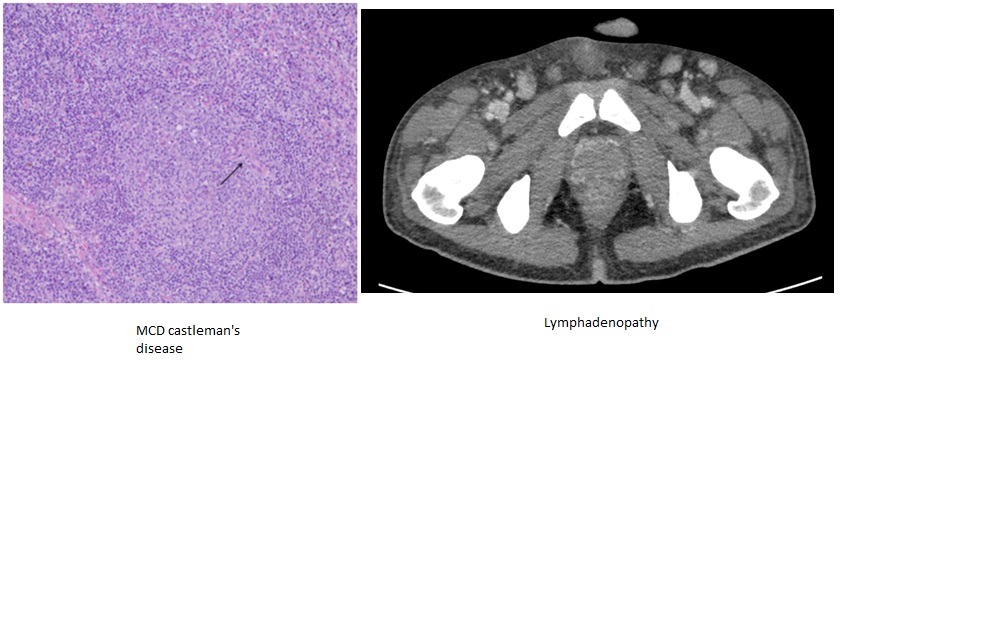
Discussion: Castleman’s disease is a lympho-proliferative malignancy that presents with a variety of systemic symptoms and lymphadenopathy of the mediastinum, mesentery, neck, axilla, and pelvis. Castleman disease can be unicentric with a discrete mass or multicentric with multiple enlarged lymph nodes. The involved nodes demonstrate unregulated proliferation of CD20+ B-lymphocytes and plasma cells. The pathology of Castleman’s disease can either be hyaline-vascular, plasma cell variant or a combination of the two. Hyaline-vascular Castleman’s disease is largely asymptomatic, while the plasma cell variant of the disease is associated with various symptoms and is often progressive. Multicentric Castleman’s disease (MCD) usually presents as the plasma cell variant, and is frequently associated to immunosuppressed states. Two more commonly associated conditions with MCD of the plasma cell variant are Human Herpes Virus 8 infection and Kaposi sarcoma, both of which were positive findings in our patient. The diagnosis of multicentric Castleman disease (MCD) is so rare that there is no accepted standard treatment today. For our patient, the discovery of Castleman disease was especially surprising given his young age. Usually MCD in HIV+ patients is most commonly diagnosed in the fourth decade of life. Rituximab is a frontrunner in recent research of MCD treatment as it is a monoclonal antibody that targets CD20+ B-lymphocytes, i.e. plasma cells. It has been increasingly used with successful survival outcomes in the plasma cell variant of MCD. Interestingly, there is some evidence to suggest that rituximab leads to progression of Kaposi sarcoma. There have not been any randomized controlled trials conducted to determine if progressive Kaposi sarcoma is related to treatment failure with rituximab.
Conclusions: This case reflects on the challenges of providing care to a patient with newly diagnosed AIDs with concurrent diseases. It is imperative to consider all diagnosis in a patient with naïve AIDs and the possibility of immune reconstitution syndrome. It also reflects on the considering MCD in HIV/AID’s patients with vast lymphadenopathy.