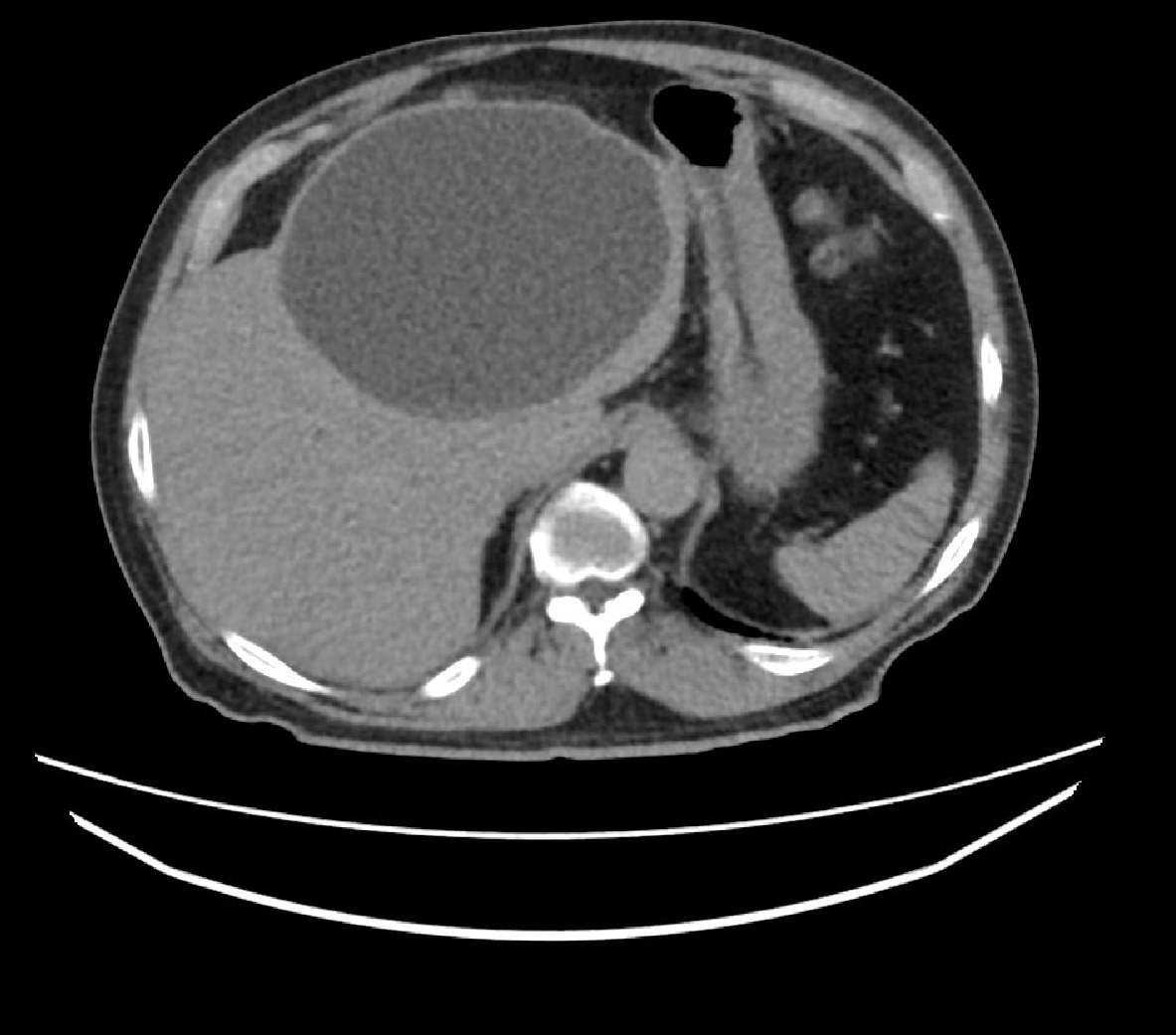
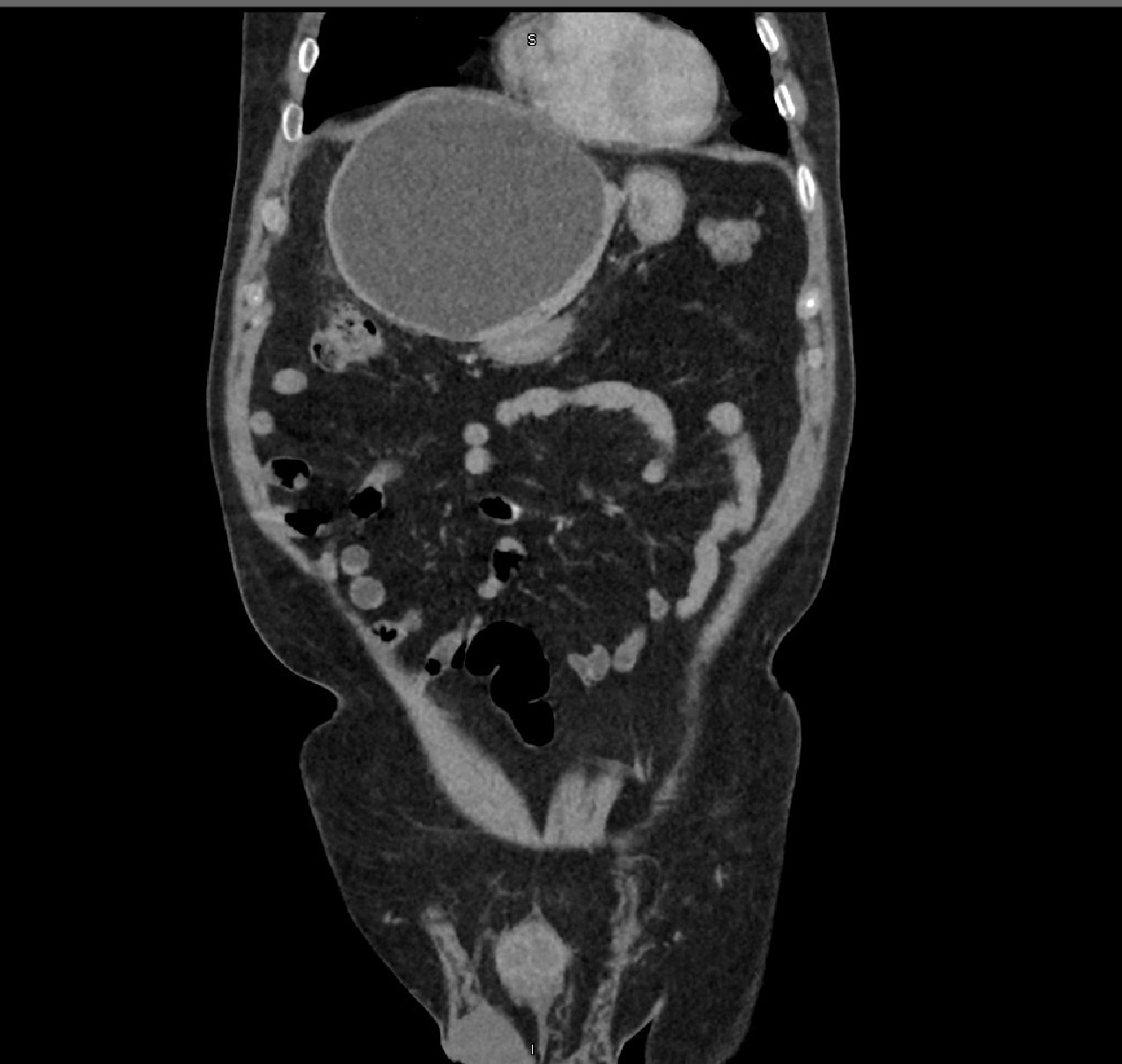
Case Presentation: A 74-year-old gentleman presented with right upper quadrant pain, nausea, fever, and chills for one-week duration. Initial workup showed simple hepatic cyst and subsequently was discharged with oral antibiotics. The patient returned a week later for persistent right upper quadrant pain and high-grade fevers. No prior history of jaundice, weight loss, intravenous drug abuse, alcoholism, or exposure to animals. On admission temperature was 100.5 °F. Physical examination was notable for right upper quadrant tenderness without rebound tenderness and negative Murphy’s sign. Laboratory findings showed WBC of 11/µl with neutrophils predominant. Liver function tests (LFTs) were unremarkable. CT abdomen showed large complex, thin-walled cystic mass, measuring 13.9 x15.3 x 13.7 cm, in the left lobe of the liver with internal echoes and varying sized septations. The initial diagnosis was pyogenic liver abscess and treated with broad-spectrum antibiotics, and cystic fluid was aspirated under fluoroscopic guidance. Patient clinically improved. Subsequently,patient developed a fever of T 99.3°F. Repeat studies showed WBC 18/µl with elevated LFTs, and negative blood cultures. New imaging showed a 14.5 x 12.3 cm fluid density mass in the left lobe of the liver, with complexities and internal debris. Patient underwent open left hepatectomy with cholcystectomy for possible cyst fenestration with liver resection. Histopathology reports came back later for biliary mucinous cystadenoma.
Discussion: The incidence of biliary cystadenoma is estimated up to 1:100,000, while the incidence of biliary cystadenocarcinoma is about 1:10 million. Both conditions are defined as cystic tumors that are lined by mucus-secreting epithelium. Recently, these two diseases have been re-defined by (WHO) to encompass one entity, classified as mucinous cystic neoplasms of the liver. Other diagnostic criteria were added, such as having an ovarian-type mesenchymal stroma or not. The reason for this new classification is due to the observation that biliary cystadenocarcinoma without ovarian stroma had a markedly worse prognosis. The clinical presentation of these tumors is highly unspecific. The most common symptom is abdominal pain and biliary obstruction, that presents in 35% of patients as obstructive jaundice, biliary colic, nausea, and fever. Some patients are even asymptomatic. Diagnosis is a challenge due to vague symptoms. Radiological evaluation is the mainstay of diagnosis. Clinicians should distinguish these tumors from simple liver cysts via the presence of internal separations and vascularity. Furthermore, studies have shown that vascularity of the septa are more specific to that of mucinous cystic neoplasm of the liver and is an essential distinguishing factor of that of a simple liver cyst. In our case, the presentation suspicious of infectious etiology, was to be managed drastically different from that of the final diagnosis. The primary treatment of mucinous cystic lesions of the liver is radical surgery.
Conclusions: Mucinous cystic neoplasms of the liver are clinically significant tumors. Diagnosis can be a challenge as clinical course mimics benign disease of infectious etiology, varied radiologic presentation, and lack of awareness of these tumors by the medical team. Radiological evaluation is currently the mainstay for a correct diagnosis, and with proper recognition of these tumors, an adequate treatment approach of radical surgical resection can be advantageous and optimizes a good prognosis.