Background: Septic arthritis (SA) of native joints has an incidence rate of 4-12 per 100,000 person-years. In 2012, there were 36, 539 hospitalizations for SA in US non-VA hospitals and costed the US healthcare system $2.85 billion. Such data has not been reported for US VA-healthcare System. SA has a mortality of 4-13%. Among survivors 1/3 experience joint deterioration. While there are clear guidelines for management of prosthetic joint SA, no such guidelines exist for native joint SA. A standard of care remains antibiotics and drainage of joint, either by medical (bedside serial needle aspiration) or surgical (arthroscopy/arthrotomy) approach, advantage of one over other unknown.
Methods: We conducted a single-center retrospective study of veterans diagnosed with SA over 10 years at a VA Hospital. Demographic, clinical, laboratory, imaging and outcome data was extracted. Inclusion criteria were positive synovial fluid culture, or synovial fluid WBC >50,000. Evaluated outcomes included joint recovery, time to recovery, sterilization of synovial fluid, need for delayed surgery, recurrence of SA in same joint, and mortality. Odds ratios were calculated by multivariate analyses for correlation of outcomes to risk factors and to management approach.
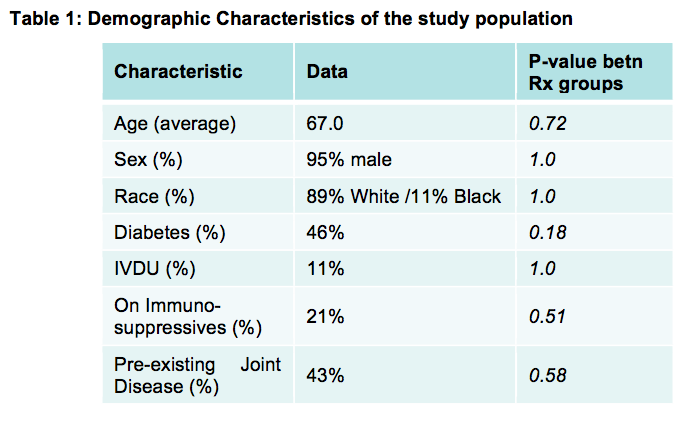
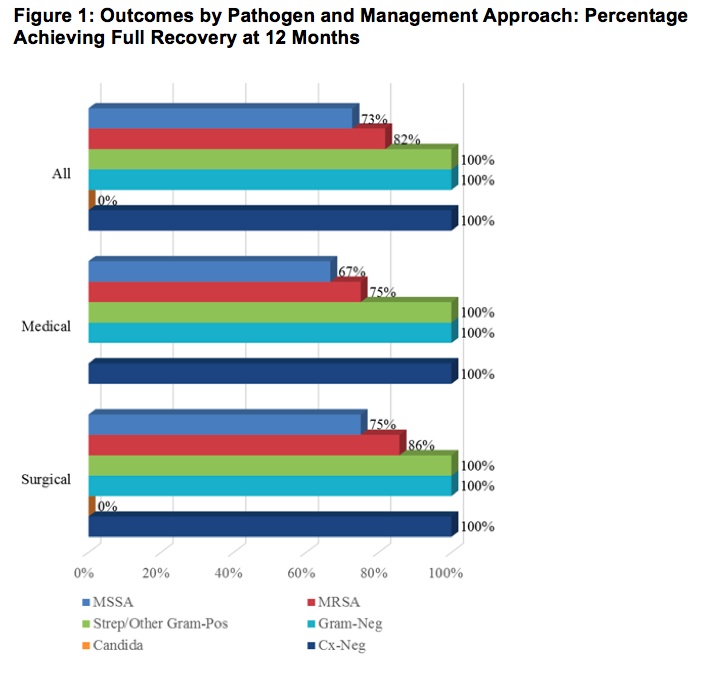
Results: Of 118 confirmed cases, 70 were in native joints and 61 met inclusion criteria. Average age was 67 years, 95% were men, 89% White, 11% Black, 46% had diabetes and 43% had pre-existing joint disease, 69% (41/61) were managed surgically (15 arthroscopy; 24 arthrotomy; 2 had both). The median length of stay for surgically managed patients was 11 days, and 13 days for medically managed (p=0.78). Median duration of antibiotics was longer in surgical group (50.1) vs medical group (35.8), (p=0.13). Staphylococcus aureus was the commonest pathogen (56% overall: 68% MSSA, 32% MRSA), followed by Streptococcus (11%) and gram-negative organisms (8%). Six (10%) patients had culture-negative SA. Of 34 patients with S. aureus SA, full recovery occurred in 8/10 medically managed (80%) and 18/24 surgically managed (75%), (p= 1.0). Mortality rate of SA was 3.2% (2 deaths total, both in surgical group). Full recovery of joint function at one year after SA was achieved equally in both groups: 15/20 medically managed (75%) and 31/41 surgically managed (76%), (p=1.0). Full recovery within 3 months was noted in 10/20 (50%) medically managed vs 8/41 (19.5%) surgically managed patients (p= 0.02). Poor outcomes were not associated with location of affected joint, causative organism, type of joint drainage, number of days to operative-room or duration of antibiotics.
Conclusions: In our single-center retrospective study, there were no statistically significant difference in outcomes at one year between patients managed medically versus surgically for septic arthritis of native joints. Full recovery at 3 months was higher among medically managed patients.