Case Presentation:
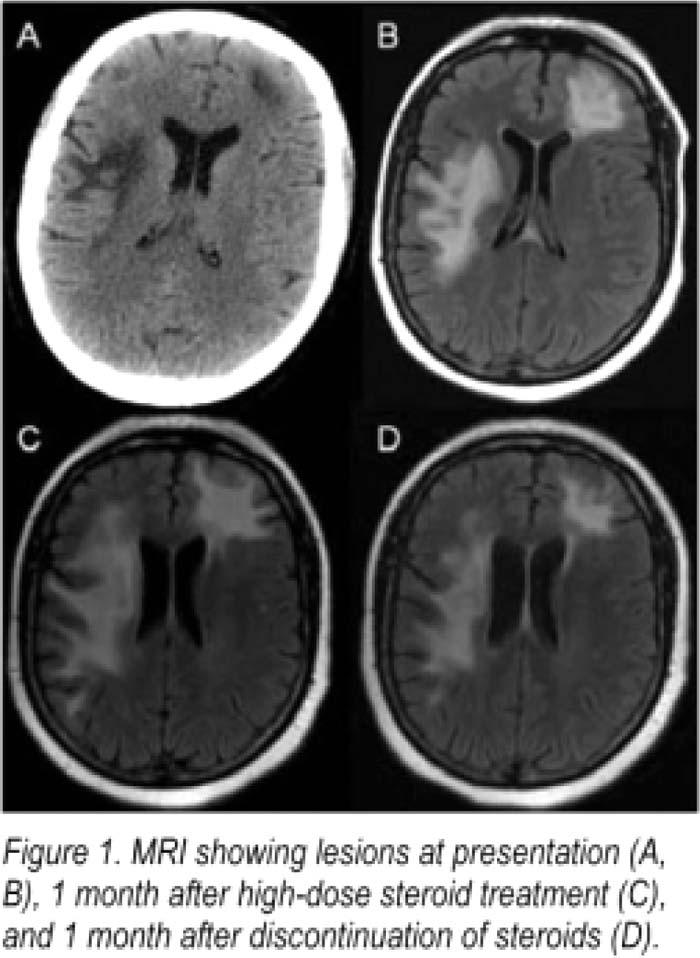
A 47‐year‐old woman presented with a 1‐week history of word‐finding difficulty, unclear speech and pareslhesias in her right leg. She denied neck pain, stiffness fever, chills, or problems with vision, memory, menlation, grasp, motor strength, or walking. Six years ago, lupus nephropathy was diagnosed and had been treated with mycophenolate mofelil and later, azathioprine. On examination, bilateral hand clumsiness was also noted. Deep tendon reflexes were a brisk 3++. She was mildly leukopenic (WBC 3.70), but chemistries, liver panel, coagulation panel, TSH, folate, and vitamin B12 were normal. CT scan showed focal hypodensities in the white matter in left frontal lobe, right parietal lobe, right temporal lobe, and right cerebellar hemisphere, suggesting a systemic process rather than an intracranial artery occlusion. MRI brain was consistent with widespread white matter disease (Fig. 1A–B). Transesophageal echocardiogram, carotid Doppler, antiphospholipid antibodies and hypercoagulable panel were negative. Elevated AMA. anti‐SSA, and anti‐Smith antibodies with decreased complements suggested lupus flare causing lupus cerebrilis. High‐dose steroids were initiated. However, her speech, walking, and balance deteriorated. MRI was repeated a month later and showed an increase in lesion size (Fig. 1C). Clinically, she was confused, had profound motor weakness, ataxic gait, and poor balance. Progression of symptoms despite treatment instigated a CSF analysis that revealed elevated JCV of 3620. thereby making the diagnosis of PML. Azathioprine was immediately discontinued and prednisone tapered. A month later JCV tiler in the CSF had reduced to 896, and MRI lesions showed a slight decrease (Fig. 1D). Her disease became stable, but some of the neurological deficits are irreversible.
Discussion:
Although PML is often considered in HIV, organ transplant, leukopenic chemotherapy and biologic (natalizumab) Therapy, and patients presenting with neurological deficits, its association with SLE is less well established. A few case reports correlating the immunosuppression in SLE with PML have been published. Clinically, PML may closely mimic lupus cerebritis, and characteristic brain MRI findings, if present, can help in their differentiation. However, if MRI lesions are nonspecific. PCR for JCV in the CSF can be extremely useful in differentiating and diagnosing PML. IT has a sensitivity of 72%–92% and specificity of 92%—100%, Early diagnosis and high index of suspicion is crucial as PML is progressive as brain remyelination does not occur in affected areas.
Conclusions:
PML should be considered in patients receiving immunomodulators for lupus management, especially in those presenting with multiple neurological symptoms or multifocal areas of white matter lesions.
Author Disclosure:
A. Verma, none: A. Moonat, none; B. J. Riskin, none.