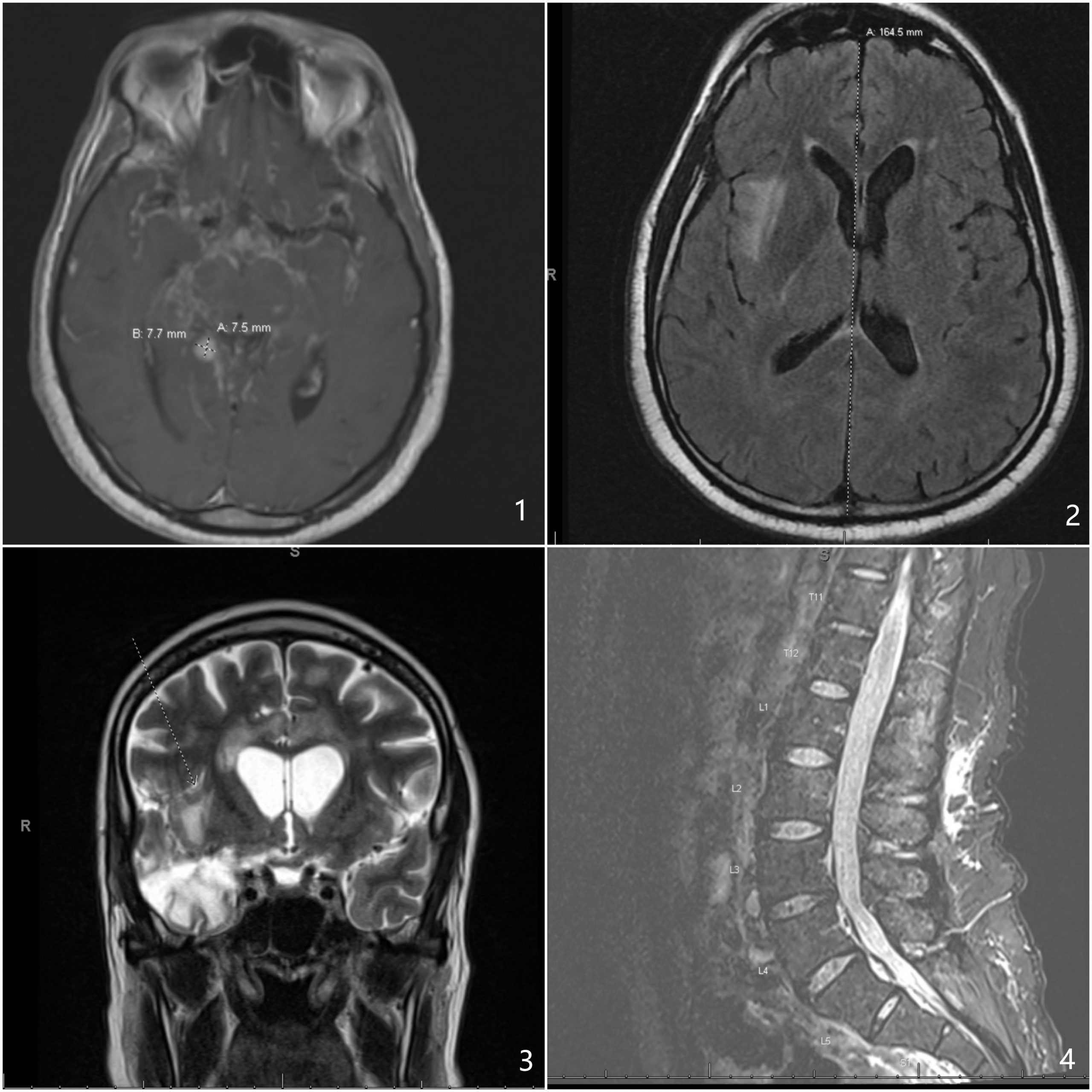
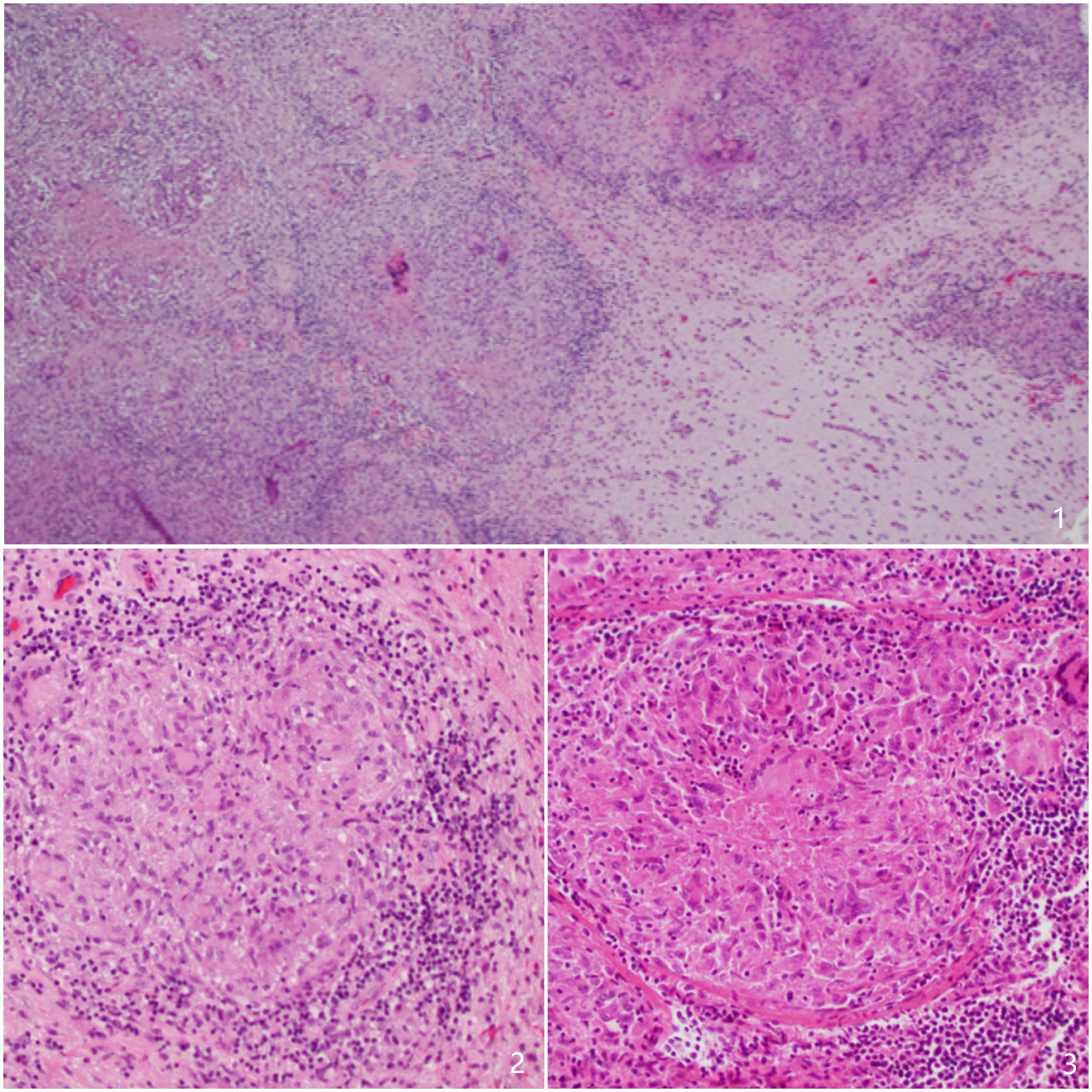
Case Presentation: 47-year-old African American incarcerated male presented with headache, new seizures, and blurry vision. Spinal fluid showed high protein, lymphocytes, mildly elevated adenosine deaminase, and low glucose. AFB, bacterial, fungal and viral studies were negative. MRI revealed severe basilar meningitis with enhancing nodular density. RIPE (Rifampicin, Isoniazid, Pyrazinamide, Ethambutol) was started, followed by RI (Rifampicin, Isoniazid) with steroid taper. He felt like “back to normal” on Infectious Disease (ID) follow-up. MRI in one month showed progression of leptomeningeal enhancement with worsening vasogenic edema. Patient required second hospitalization due to confusion. Differentials were broadened including CNS lymphoma, sarcoidosis (considered less likely without pulmonary involvement). CSF AFB smear remained negative. Brain biopsy was reported as “chronic necrotizing granulomatous inflammation, favors an infectious etiology however special stains for mycobacterial and fungal organisms are negative”. Based on history and pathology report, TB was prioritized over neurosarcoidosis. He was discharged on RPEL (Rifampin, Pyrazinamide, Ethambutol, Levofloxacin) for suspected MDR (multi-drug-resistant) TB. He was followed by a new ID physician with stable repeat MRI. In the next few months patient had worsening lower extremities weakness with poor balance, then wheelchair bound. Repeat MRI showed new 6-8 mm enhancement in frontal area with surrounding edema, stable leptomeningeal enhancement. RPEL was continued. Repeat MRI in 6 months showed signs for reactivation of disease, and enhancement throughout thecal sac, raising concern for new tuberculoma or unresponsiveness to RPEL, prompting 3rd hospitalization. CSF again did not show AFB or other causes. RPEL was stopped. A review of previous brain biopsy with another pathologist revealed focal debris consistent with non-necrotizing granulomas, which can be seen in both sarcoidosis and mycobacterial disease, though not pathognomonic for sarcoidosis.[1] A review of previous inguinal biopsy showed a T-cell CD4: CD8 ratio near 8:1, relatively specific for sarcoid.[2] Considering lack of improvement and development of new lesion despite MDR TB treatment, neurosarcoidosis was finally prioritized. Patient was started on high dose steroids followed by mycophenolate. Mentation improved and he was discharged with close neurology follow-up.
Discussion: Sarcoidosis is an idiopathic multi-system disorder.[3] The incidence of isolated central nervous system involvement is less than 1%.[4], [5] The complexity of clinical, radiographical and pathological presentations pose a significant diagnostic challenge.[6] This case, we saw a rare case of neurosarcoidosis with delayed diagnosis. Sarcoidosis mimics various conditions.[7] Here, numerous tests failed to identify any infectious organisms. However, patient was treated for TB for 17 months. The social history of incarceration, pathology reports of “necrotizing granuloma”, with change of key ID physician during the 2nd follow-up could have all contributed to anchoring bias[8] and premature closure[9].
Conclusions: Recognizing the nuance of pathology interpretation, neurological symptoms[10], a holistic approach towards clinical picture could have curbed cognitive biases, leading to a timelier diagnosis and better outcome. [11]