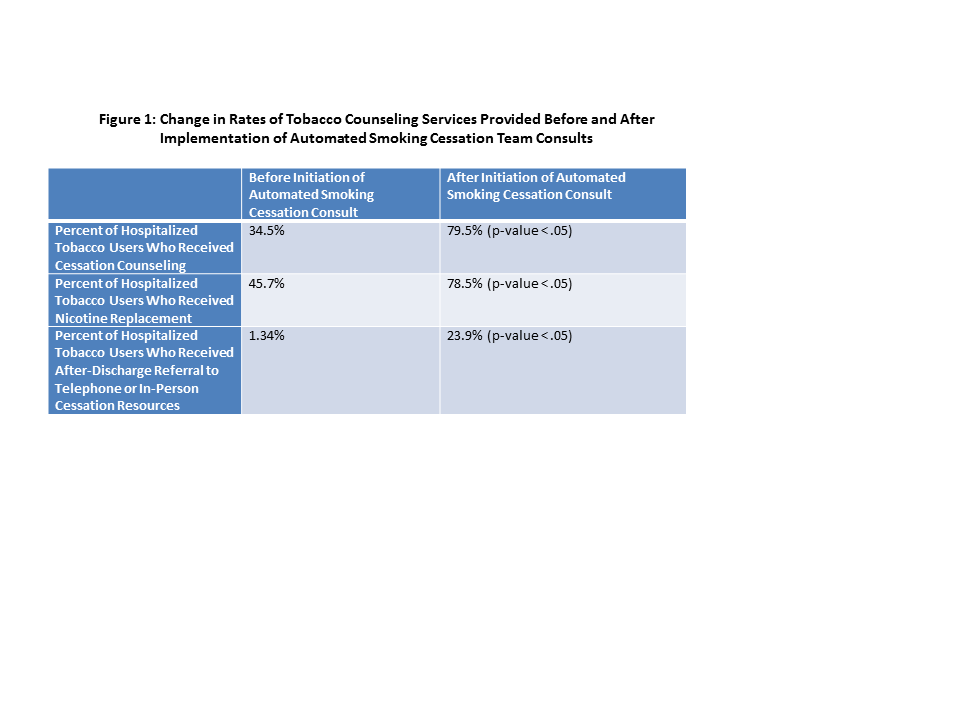
Background: Inpatient hospitalization represents a key time for patients who use tobacco to quit smoking, and inpatients who receive smoking cessation counseling, nicotine replacement, and referral to outpatient resources have increased quit rates six weeks after hospital discharge. However, in 2014, only 34.5% of tobacco users admitted to our 600-bed academic hospital were documented as having received and accepted tobacco cessation counseling, only 45.7% of tobacco users received nicotine replacement therapy, and only 1.35% of tobacco users received after-discharge consultations to outpatient smoking cessation resources.
Methods: At our hospital, tobacco use is documented when the admitting nurse asks the patient about tobacco use status during the nursing admission assessment and documents this result in the social history tab of the electronic health-record. Physicians, pharmacists, and nurses may also subsequently update the tobacco use status under the social history tab. We piloted a system in which a dedicated Respiratory Therapist-staffed Smoking Cessation Consult Service was trained to provide targeted tobacco cessation services to all inpatients who use tobacco. We implemented a system to link each inpatient’s tobacco use status to the Smoking Cessation Team Consult list, so that all patients with documented tobacco use automatically populates the Smoking Cessation Team Consult list.
The Respiratory Therapist-staffed Smoking Cessation Consult Service received a day-long training session focused on providing tobacco cessation counseling through motivational interviewing and pharmacotherapy for tobacco cessation provided by faculty from the University of California at San Francisco and the Mayo Clinic Nicotine Dependence Center. A Smoking Cessation Consult consists of an initial visit to the inpatient for motivational interviewing and cessation counseling and initiation of nicotine replacement if desired by the patient, and a second visit that includes further counseling and follow-up, and referral to either a telephone quit line or outpatient smoking cessation center. All nicotine replacement orders initiated by a Respiratory Therapist need to be co-signed by a physician, and the referrals to outpatient smoking cessation services are electronic referrals and provide electronic feedback about the patients’ progress that is available in the electronic health-record.
After six months, we queried our Epic-based EHR with a customized report to determine what percentage of patients who use tobacco received cessation counseling, nicotine replacement, and referrals to outpatient cessation resources before and after the implementation of the automated Smoking Cessation Team Consultation Service.
Results: After initiation of automated consults to the Smoking Cessation Team for all patients who use tobacco in the hospital, of 1944 patients identified as using tobacco, 1545 received and accepted cessation counseling from a trained member of the Smoking Cessation Team, 1526 received nicotine replacement therapy, and 464 received an electronic referral to either a telephone or in-person quit line (Figure 1).
Conclusions: An automated system for providing smoking cessation services to all inpatients expedites the provision of cessation counseling, nicotine replacement, and referral to outpatient resources. Further study is ongoing to determine whether automated smoking cessation consults lead to increased rates of cessation after discharge.