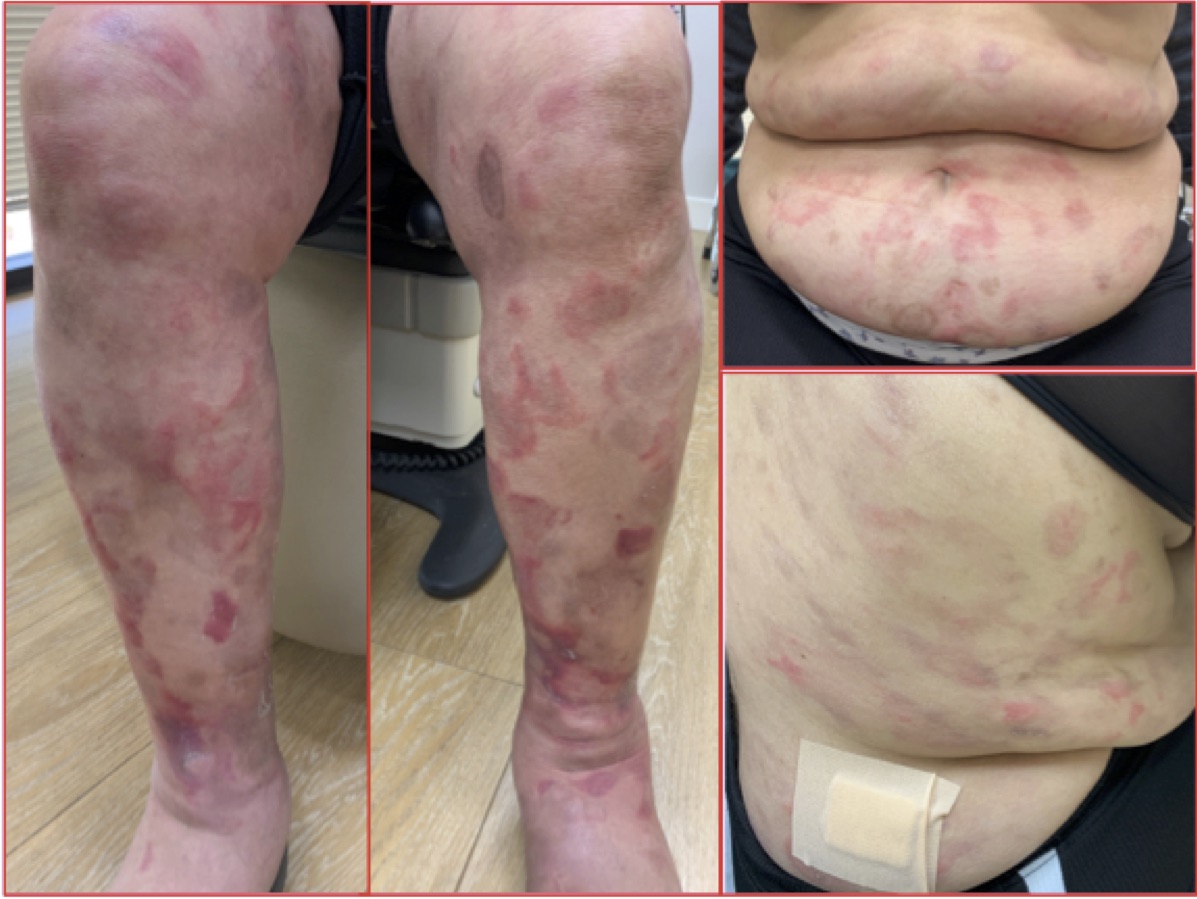
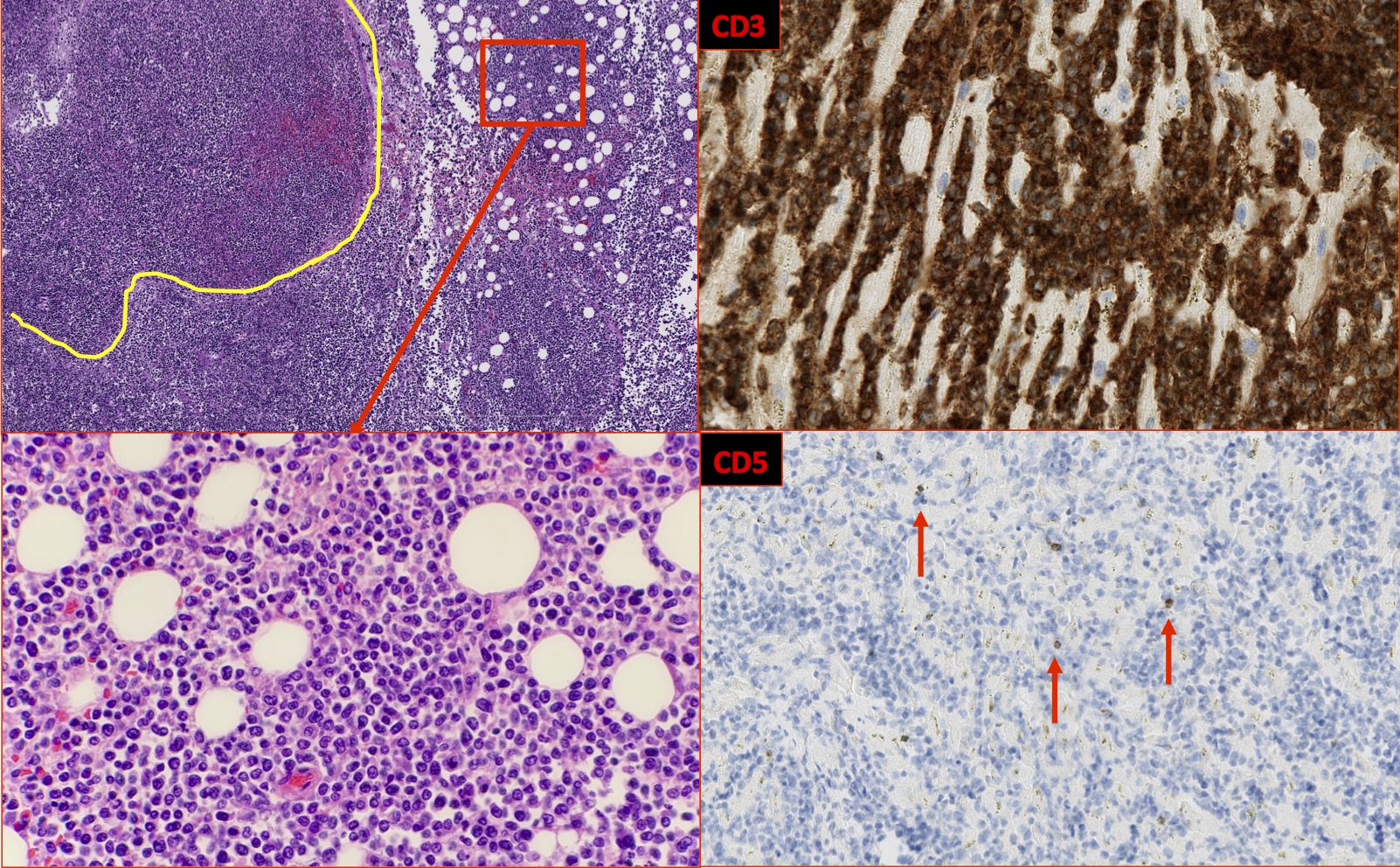
Case Presentation: A 60-year-old, Guatemalan female without prior medical history presented with a transient, erythematous, burning, rash involving her extremities and torso (Figure 1). Additional symptoms included fatigue, chills, joint pain, early satiety and weight loss. Blood counts, metabolic panel and serum protein electrophoresis were normal. C-reactive protein (13 mg/L, normal (N) <10 mg/L) and rheumatoid factor IgG (87.3 mg/dL, N <25 mg/dL) were elevated. Rheumatology workup was otherwise negative. Skin biopsy revealed mildly dense neutrophilic and eosinophilic infiltrate. Steroids improved the rash. A malignancy workup was recommended but not completed due to fear of coming to clinic during the COVID-19 pandemic. Six months later, the patient re-presented with back pain, abdominal distention and shortness of breath. Rash had resolved and 2+ edema was present. Laboratory results included: leukocytosis (WBC 15 k/uL, N 4.5-11 k/uL), thrombocytopenia (plt 106 k/uL, N 140-440 k/uL) and elevated liver function tests (AST 127 U/L, N 12-25 U/L; ALT 262 U/L, N 11-53 U/L), alkaline phosphatase (399 U/L, N 24-118 U/L), creatinine (1.59 mg/dL, N 0.5-1.2 mg/dL) and lactic dehydrogenase (1045 U/L, N 98-192 U/L). CT imaging showed pulmonary infiltrates, hepatomegaly and a mesenteric mass with lymphadenopathy. MRI showed no evidence of the mass. The patient decompensated over 48 hours. She developed lactic acidosis and leukocytosis. She required pressor support, mechanical ventilation and renal replacement. Labs were consistent with disseminated intravascular coagulation (DIC). Blood cultures grew Candida albicans and the patient died despite antifungals. An autopsy revealed a mesenteric mass and significant lymphadenopathy. Pathology was consistent with disseminated peripheral T-cell lymphoma-not otherwise specified (PTCL-NOS) (Figure 2).
Discussion: This case was concerning for malignancy given the unexplained weight loss, new rash and lab abnormalities. Tissue diagnosis was impaired due to poor follow up, discrepant imaging studies and rapid demise. PTCL comprises a rare, heterogeneous group of aggressive neoplasms, accounting for 15% of all non-Hodgkin lymphomas [1]. The majority (69%) of patients present with an advanced stage and 5-year survival is 32% [1]. Common presenting symptoms include lymphadenopathy with variable extranodal disease involvement [1]. 44% of patients have B-symptoms (fatigue, weight loss, fever, night sweats) [1]. At presentation anemia and/or thrombocytopenia are present in 25% of patients and LDH is elevated in 50% [1]. Concurrent presentation of skin and systemic disease in PTCL-NOS has been rarely described [2]. A study of 15 patients found rash had variable morphology and involved the trunk (33%) and lower extremities (47%). Like this case, immunophenotype was CD3(+) (100%), CD8(-) (100%) and CD4(-) (33%) [2]. Unlike this case, skin biopsy revealed T-cell infiltrate [2]. Disseminated PTCL-NOS may have predisposed the patient to candidiasis. Candidemia has 30-40% mortality despite treatment [3]. Septic shock likely precipitated DIC, contributing to decompensation [3].
Conclusions: Learning objectives include: recognize rash may be an atypical presentation of lymphoma, evaluate discrepant imaging results, obtain tissue biopsy in malignancy evaluation, and understand PTCL as a disease that presents with nonspecific symptoms, often at a late stage with a poor prognosis. Especially during the COVID-19 pandemic, patients may present at later stages.