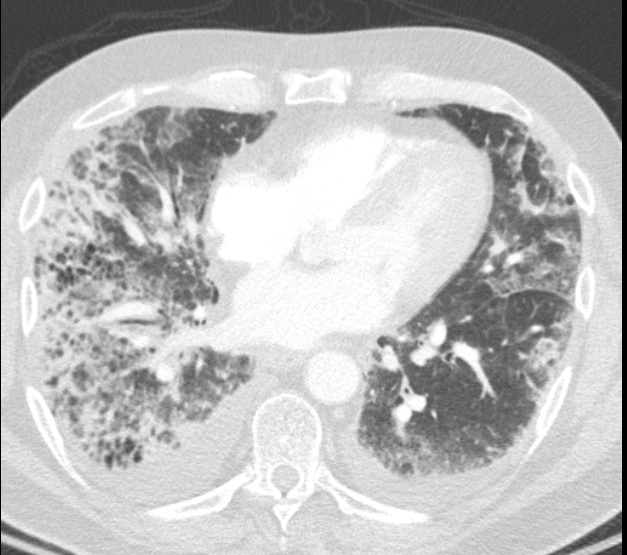
Case Presentation: A 65 year-old man was admitted to the inpatient medical service with worsening cough and dyspnea. He also reported progressive muscle weakness and myalgias over the past several weeks. His past medical history was significant for tobacco use, hypertension, hypothyroidism, and obesity. On admission, he was hemodynamically stable and afebrile with mild tachypnea and hypoxia. Physical exam revealed diminished breath sounds with rhonchi in the right lung fields, diffuse erythematous rash over his anterior chest, and reduced extremity strength. Initial laboratory evaluation showed WBC 9.9 with remainder of CBC unremarkable, normal creatinine and electrolytes, creatinine kinase 4100, albumin 2.9, CRP 57, ALT 90, and AST 233. Chest x-ray was notable for consolidation in the right lower lobe. He was treated with antibiotics and supportive care for presumed community-acquired pneumonia. However, over the next several days he clinically worsened and unfortunately developed hypoxic respiratory failure requiring ICU admission. CT chest showed extensive reticular opacities, most prominent in the bases, with areas of honeycombing more advanced in the right lung. Muscle biopsy was done, with pathology findings consistent with dermatomyositis. He was thus diagnosed with dermatomyositis with antisynthetase syndrome and associated interstitial lung disease (ILD). He was started on high dose steroids, immunosuppression with cyclophosphamide, and later plasmapheresis. He subsequently made significant respiratory and systemic clinical improvement, although he did require long-term oxygen supplementation and multiple hospital admissions.
Discussion: Dermatomyositis can have acute, life-threatening multisystem manifestations, particularly in cases with associated antisynthetase syndrome. This is caused by antibodies to aminoacyl-transfer ribonucleic acid (tRNA) synthetase enzymes. Antisynthetase syndrome is characterized by severe, rapid-onset interstitial lung disease which can cause respiratory failure, polymyalgias and arthritis, and Raynaud’s phenomenon. Anti-Jo-1 antibody serologies are often positive in these patients but are not necessary for diagnosis, and in fact were negative in this patient’s case. First-line treatments include steroids and immune suppression such as cyclophosphamide. In very severe cases, plasmapheresis can also be used. Additionally, dermatomyositis often weakens the upper third (striated) portion of the esophagus, predisposing patients to aspiration and therefore additional pulmonary complications.
Conclusions: Interstitial lung disease, although much less common than other inpatient pulmonary conditions such as pneumonia, is an important cause of acute hypoxic respiratory failure encountered by hospitalists. ILD associated with antisynthetase syndrome in the setting of dermatomyositis is often particularly aggressive, and therefore prompt diagnosis and treatment by the inpatient team is essential.