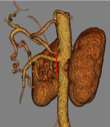
Case Presentation: A 54-year-old male with alcoholic cirrhosis and type 2 diabetes presented to the hospital for 2 weeks of recurrent syncopal episodes. One year prior to presentation, he underwent EGD to work-up chronic intermittent nausea, abdominal pain, bloating, and heartburn; this was unremarkable. Colonoscopy showed non-bleeding internal hemorrhoids and few diverticula. One month prior to presentation, he underwent CT abdomen and pelvis for hepatocellular carcinoma screening; this revealed cirrhosis and narrowing of the proximal celiac artery by median arcuate ligament compression. At presentation, he described 3 syncopal episodes without prodrome over the preceding two weeks.He was afebrile, orthostatic, tachycardic (100 bpm), and hypoxic (4 L/min supplemental oxygen to maintain a saturation >90%). Labs revealed a leukocytosis (16.9 /mm3; reference range [RR] 4,500-11,000 /mm3), and otherwise unremarkable CBC, CMP, TSH, and troponin. EKG showed no pathology. Chest CTA showed bibasilar infiltrates concerning for aspiration. He was cultured and started on empiric antibiotics. During admission, telemetry, spot EEG, and echocardiography were normal. His hypoxia improved with antibiotics and supportive care. CT mesenteric ischemia protocol showed marked stenosis and hooked appearance of the proximal celiac trunk from compression by the median arcuate ligament (Figure 1). A HIDA scan was normal. He was diagnosed with median arcuate ligament syndrome (MALS) with plans to undergo outpatient surgical planning. His syncope was from hypoxia secondary to aspiration pneumonia / pneumonitis related to MALS-induced vomiting.
Discussion: MALS is a rare condition in which the MAL compresses the celiac axis and/or ganglion.1 Individuals with a more cephalad celiac origin and/or a more caudad MAL are at risk of compression of the celiac artery (Figure 2).1 Pathophysiology is unclear, but hypotheses include: 1) foregut ischemia from a compressed celiac artery; 2) chronic compression of the celiac ganglion; 3) diverted blood flow through large collateral vessels causes symptoms in individuals with an occluded or compressed celiac trunk.2,3 MALS presents with nausea and vomiting, postprandial epigastric pain, bloating, and unintentional weight loss. Affected individuals often undergo extensive evaluation prior to the diagnosis. Confirmation of celiac stenosis is made by duplex ultrasonography, abdominal CT or magnetic resonance (MR) angiography, or angiography of the celiac artery.1,4 Treatment involves open surgical decompression +/- reconstruction or laparoscopic or robotic MAL release +/- ganglionectomy.2,5-9 Percutaneous transluminal angioplasty +/- balloon-expandable stent is often considered with post-surgical residual symptoms.10 Enteric bypass may be considered for persistent symptoms.
Conclusions: MALS is rare and requires a high index of suspicion in patients with symptoms of chronic nausea and vomiting, postprandial epigastric pain, bloating, and unintentional weight loss. It is a diagnosis of exclusion often established after an extensive work-up. The general internist should be familiar with this condition and have a low threshold to pursue celiac artery imaging modalities in suspected cases.