Background: Hospitals are facing increasing pressure to optimize throughput in order to reduce excess length of stay and improve emergency department (ED) boarding times. Improving coordination and throughput in complex organizations with multiple care sites can be particularly challenging. Health systems have implemented numerous initiatives to improve hospital throughput, but these efforts have mainly been focused in the ED.
Purpose: We implemented a trans-disciplinary “Flow Control Team” (FCT) aimed at methodically identifying and mitigating real-time barriers to throughput for hospitalized patients.
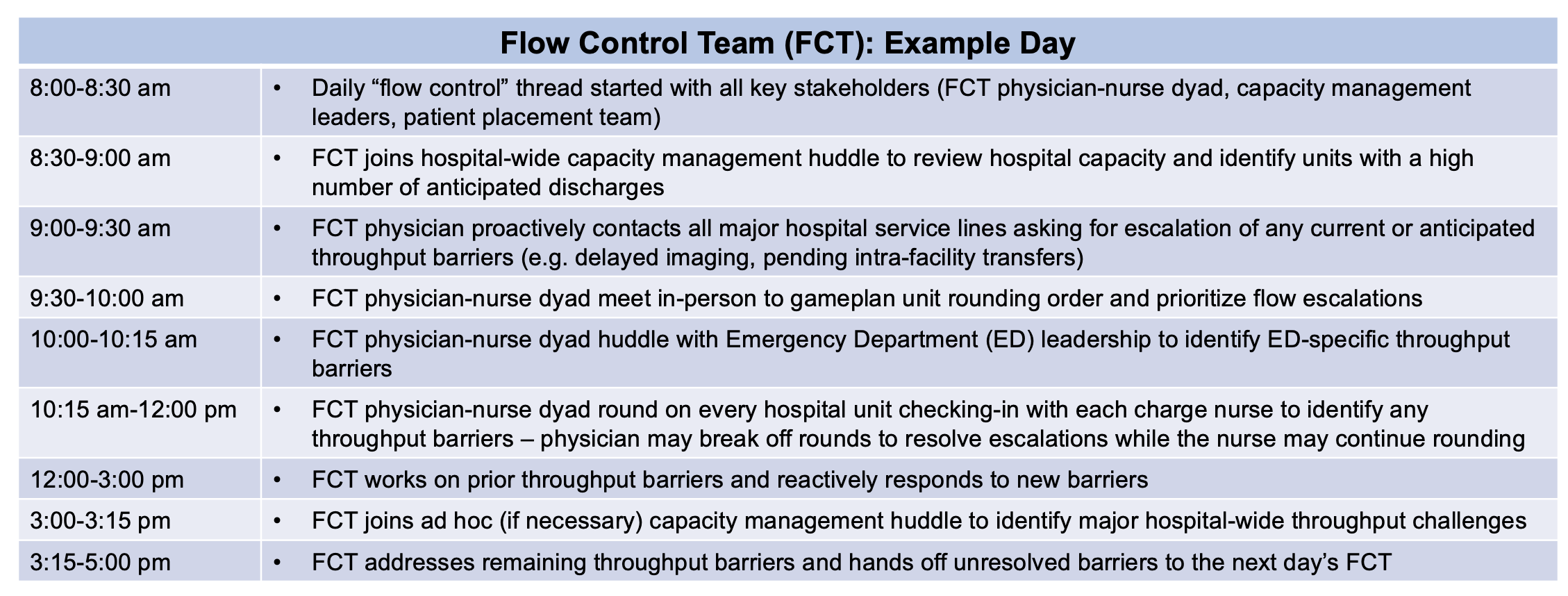
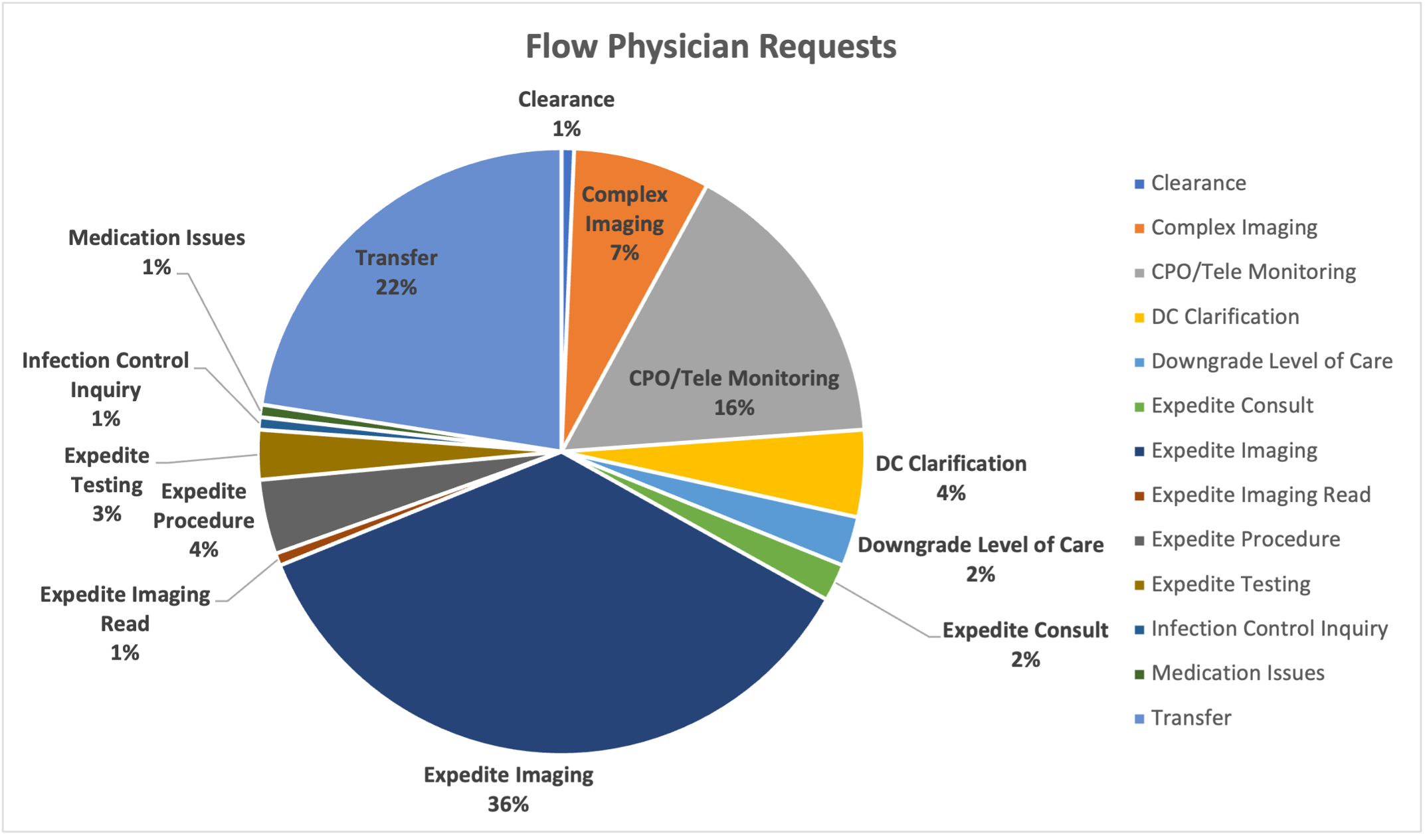
Description: The FCT launched September 2021 at a large, urban 652-bed academic medical center which operates at an average staffed beds occupancy of 90% and has three adult inpatient care sites. The FCT concept was modeled after similar teams from partner academic medical centers with the primary goal of identifying and assisting with barriers to discharging patients from the adult hospital units. This spawned from a larger health systems effort to improve hospital capacity. The FCT was comprised of a physician-nurse dyad and was supported with administrative assistance from the patient placement department. Physicians from across all specialties were recruited and paid a fixed rate for each nine-hour shift. The majority were hospitalists, with additional representation from emergency medicine, critical care, and neurology. FCT nurses were drawn from the hospital supervisor group and primarily monitored unit-level staffing needs based on anticipated capacity. Funding was provided by the health system. The FCT was available all non-holiday weekdays and the annual cost of the program was estimated to be ~$400,000 for 2022.Responsibilities of the FCT were to proactively contact charge nurses and primary medical and surgical teams to identify discharge barriers, care delays, and opportunities for transfers out of the primary hospital. The FCT then worked with hospital/system level supervisors to expedite evaluation and management (Figure 1). FCTs worked closely with supervisors in Radiology, Anesthesia, Cardiology, Case Management, Patient Placement, Physical/Occupation Therapy and Pharmacy. FCT physicians could also be contacted directly by hospital or ED teams to assist with needs not identified during morning rounds. In a review of 16 FCT days, the FCT was contacted about an average of 10 patients per day, with the most common requests being to help expedite imaging studies (36%), decrease unnecessary safety monitoring (16%), and facilitate transfers from the primary hospital to secondary sites (22%) (Figure 2). Additional requests included high-effort operational tasks (e.g. transferring patients offsite for complex imaging studies), expediting procedure scheduling, and addressing time-sensitive discharge barriers (e.g. expediting COVID tests for facility placement). In a survey of 28 attending hospitalists, 77% had positive feedback on the program, reporting that the FCT successfully resolved or expedited their issue, helped to facilitate earlier discharge times, increased intra-facility transfers, reduced length-of-stay, and reduced excess hospital days.
Conclusions: The FCT aimed to identify and resolve throughput delays in real-time, and initial data suggest that this program is helpful to inpatient physicians. A hospital flow control team staffed by clinicians empowered to remove discharge barriers may be a replicable model that can improve hospital throughput.