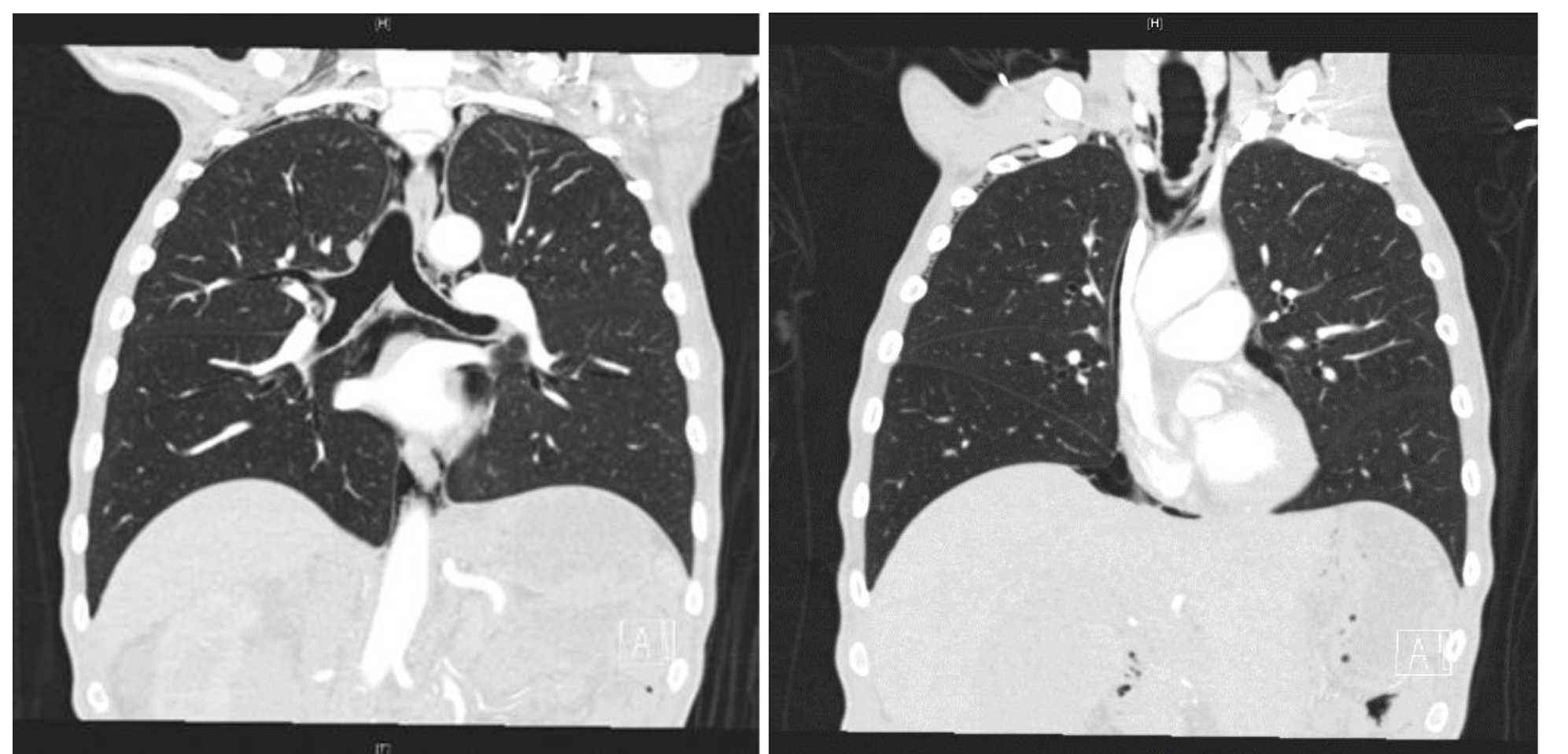
Case Presentation: A 58-year-old man was brought to the emergency room by his friend for self-neglect. Approximately one year ago, the patient’s mother died. He has been afraid to eat since. Instead, nutritional intake was exclusively liquid and consisted of water, Gatorade and Boost meal supplement. He lost 200 pounds over the past year. Somatic complaints included orthopnea and dry throat. In the emergency room, the patient was disheveled, covered in feces and dried urine. Blood pressure was 108/80, pulse 100 bpm, and respiratory rate was 18 breaths per minute. Pulse oximetry was 99% and he was afebrile. He was cachectic, with temporal wasting, scaphoid abdomen, bilateral arm edema and redundant skin folds. He had no focal weakness and was unable to lift himself up in bed. CT Imaging revealed extensive pneumomediastinum, tiny pneumothorax, pneumoperitoneum, anasarca with mesenteric edema, and rectal and sigmoid wall thickening, concerning for proctocolitis. CTA revealed widely patent SMA and IMA, and no evidence of superior mesenteric venous thrombosis. Parenteral nutrition was initiated. Esophagram ruled out perforation. General and Thoracic Surgery services determined that no surgical intervention was indicated. They recommended starting enteral feeds and avoiding antibiotics. Patient refused an endoscopic gastrointestinal evaluation. Psychiatry service concluded patient had a “feared complaint with no diagnosis.” On day 4, plain films revealed improvement in pneumomediastinum. He was ultimately discharged to a skilled nursing facility.
Discussion: Diffuse pneumomediastinum, pneumothorax and pneumoperitoneum in the absence of barotrauma (e.g., positive pressure ventilation or vomiting), infection or chronic obstructive lung disease is uncommon. Emphysema due to severe malnutrition was hypothesized in World War II autopsy reports of civilian casualties. In 2004, Coxson et al compared chest CT and spirometry results from twenty-one patients with anorexia nervosa to sixteen patients without anorexia or chronic lung disease. Measured CT lung density and mean volume of gas per weight of lung tissue were significantly lower in patients with anorexia, suggesting early emphysema-like changes. Serum α1 antitrypsin levels were normal in both groups. In 2009, Gardenghi et al reported diminished and progressive DLCO values in twenty-seven patients with anorexia, stratified by duration of disease. The data also revealed diminished respiratory muscle strength in patients with anorexia. Malnutrition-induced surfactant deficiency and low glycogen stores may explain these findings but have not been directly tested. Animal studies suggest that these structural changes are reversible with improved nutrition.
Conclusions: We present a case of severe malnutrition due to self-neglect complicated by pneumothorax with resultant pneumomediastinum and pneumoperitoneum. Care provided included prompt nutritional therapy to help reverse the structural changes associated with long term starvation. This also required close surveillance for refeeding syndrome, arrythmias and pressure related skin breakdown, as well as addressing the underlying psychiatric or inflammatory cause.