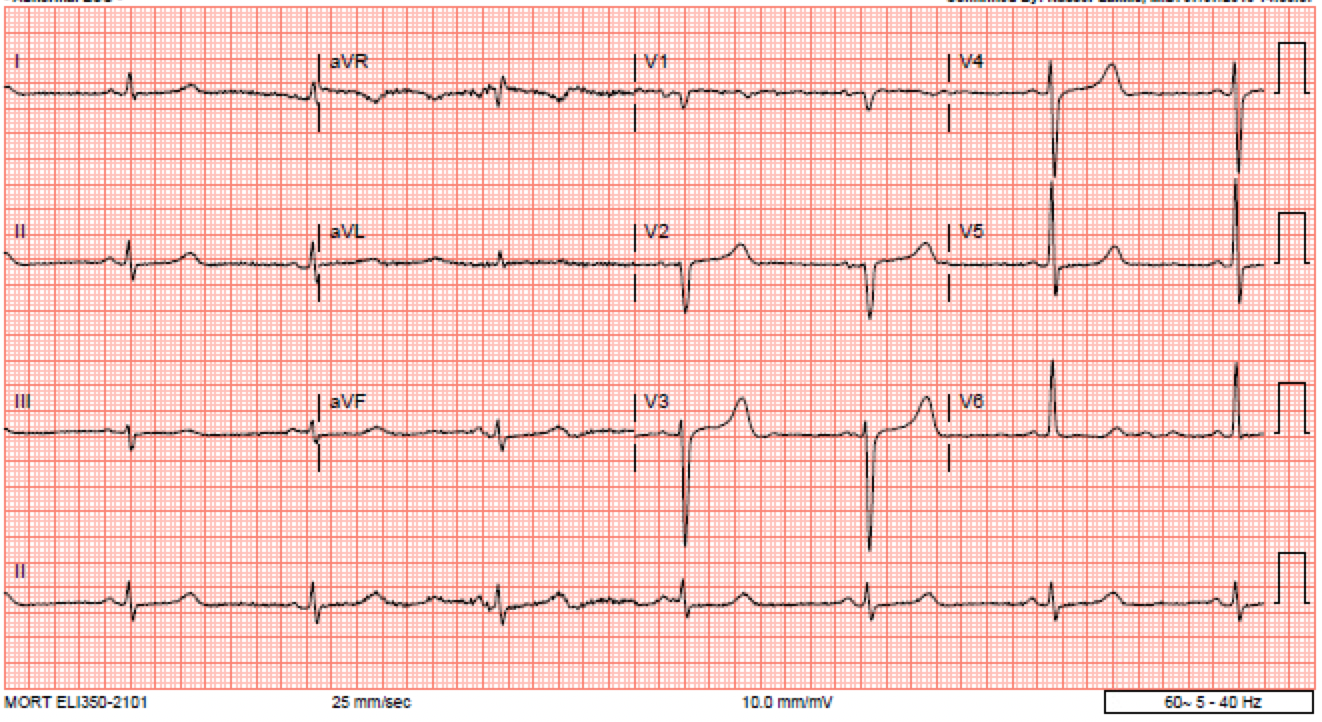
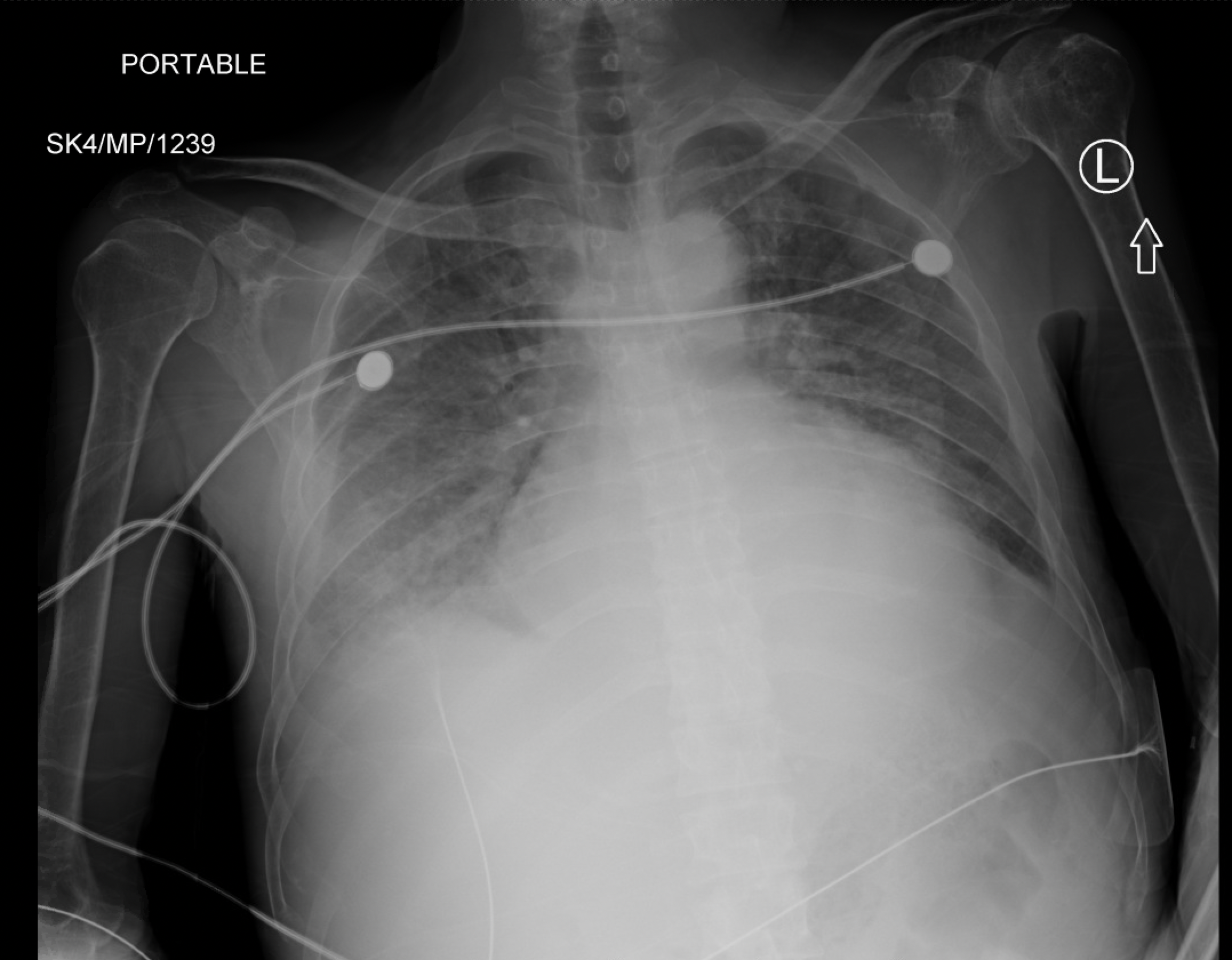
Case Presentation: Hypermagnesemia is a rare but serious condition associated with impaired renal function. We report a case of bradycardia with hypothermia secondary to hypermagnesemia from consumption of milk of magnesia (MgOH2) in a patient with end-stage kidney disease (ESKD). A 52-year-old man with ESKD on emergent hemodialysis, diabetes mellitus, hypertension, and hyperlipidemia presented for chest pain and fatigue over the preceding 24 hours. His medications include insulin and carvedilol, the last known doses of which were 3 days and 1 day prior, respectively, and he had ingested unspecified but excessive doses of milk of magnesia for gastrointestinal distress in the days leading up to hospitalization. Vital signs were notable for bradycardia to 41/min and blood pressure of 135/67 mmHg with development of hypothermia to 33.9 ℃ (93℉) during the course of the diagnostic workup. Physical examination showed lethargy and crackles in the lower lung fields bilaterally. Electrocardiogram showed sinus bradycardia with prolonged QTc interval (500 msec), and chest radiography showed bilateral pulmonary edema consistent with volume overload. Laboratory studies were notable for serum magnesium of 5.6 mg/dL. Hemodialysis was initiated for definitive treatment of symptomatic hypermagnesemia. His bradycardia resolved after one dialysis session and his hypothermia resolved after the second session, bringing his magnesium level down to 2.9 mg/dL. He was discharged to home in stable condition and cautioned to avoid magnesium-containing medications in the future.
Discussion: Magnesium is an intracellular divalent cation that plays an essential role in nerve conduction, muscle contraction, vascular tone, and cardiac conduction. Less than 1% of total body magnesium is found in blood. Serum concentrations >2.6 mg/dL are considered hypermagnesemic and symptoms typically manifest at >3.6 mg/dL. Signs of hypermagnesemia include lethargy, diminished reflexes, respiratory depression, impaired thermoregulation, bradycardia, and cardiac arrest. Because the kidney is a major regulator of magnesium homeostasis, patients with ESKD are vulnerable to developing hypermagnesemia even with therapeutic doses of magnesium-containing supplements. Treatment options include excretion of magnesium via loop or thiazide diuretics, antagonism of magnesium via calcium, and direct removal of magnesium from blood via hemodialysis in more severe cases. For our acutely symptomatic patient whose last session of emergent dialysis was a week prior, dialysis was the treatment of choice.
Conclusions: It is important for clinicians to educate patients with ESKD on their increased susceptibility to magnesium toxicity from magnesium-containing laxatives or supplements. Furthermore, clinicians should consider hypermagnesemia in their differential for patients with renal dysfunction presenting with bradycardia, altered mental status, and hypothermia. If symptoms are severe, hemodialysis can rapidly correct the serum magnesium concentration, reducing the patients’ risk of fatal arrhythmias.