Background: As the United States population ages the health care system is experiencing overall change and growth in the patient population as evidenced by the rising demand of psychiatric care in the emergency department. By the year 2029 “baby boomers” or older adults, those born between mid-1946 through mid-1964, will be 65 and older resulting in 20 percent of the total U.S. population to be greater than 65. This study aims to identify factors in the older adult that may contribute to involuntary hold status in the ED.
Methods: This study is a retrospective review conducted at a suburban acute-care hospital ED of adult patients evaluated while on involuntary hold from January 1, 2014, through November 30, 2015. Data collected included age, date of birth, sex, race, marital status, housing, payer source, and tobacco use. Clinical data collected included ED length of stay, reason for involuntary hold, psychiatric disorder, suicide attempt, substance use disorder, serum alcohol level, urine drug testing, medical comorbidity, violence in the ED, 30-day ED readmission, and 30-day mortality. To compare the older adults (patients born in 1964 or before) to younger adults (born 1965 or after), categorical variables were evaluated using the Pearson χ2 test and the Fisher exact test and continuous variables were evaluated using the Wilcoxon rank sum test.
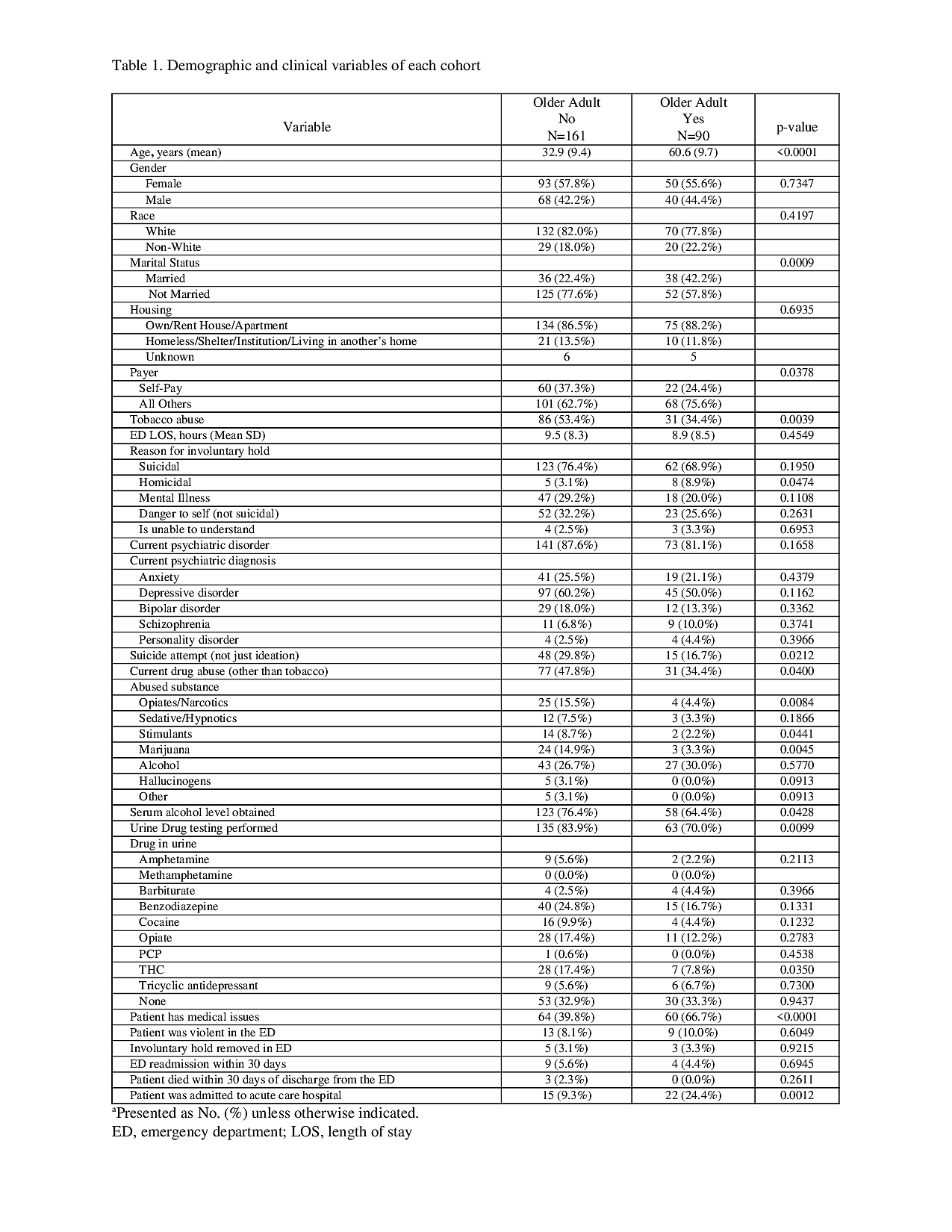
Results: Two-hundred and fifty-one patients were included in the study. Of these, 90 (35.9 %) were classified as older adults with an average age of 60.6 years and 161 (64.1 %) were younger adults with average age of 32.9 years. The most common reason for involuntary hold in both cohorts was suicidal ideation. Medical comorbidities were more prevalent in older adults [60 (66.7%) vs. 64 (39.8%), P=<0.0001] resulting in greater need for acute care hospital admission [22 (24.4 %) vs. 15 (9.3 %), p=.0012]. Older adults were more likely to be non-smokers [59 (65.6%) vs. 75 (46.6 %), P=0.0039] and overall were less likely to have current drug abuse [31 (34.4 %) vs. 77 (47.8 %), P=0.04]. Older adults underwent less serum alcohol testing [58 (64.4%) vs 123 (76.4%), p =0.04] and urine drug testing [63 (70.0%) vs. 135 (83.9%), p=0.01]. Cohorts were not significantly different with respect to sex, race, violence in the ED, psychiatric diagnosis, and ED LOS. (Table 1).
Conclusions: Involuntary older adult patients have unique characteristics that may present challenges in their care and transfer of care to the inpatient psychiatric facility. When compared to younger adults, they are less likely to use drugs. However, the older adult often presents with medical comorbidities that require hospitalization and may exacerbate their underlying psychiatric illness. Increasing awareness of underlying comorbidities may assist in more readily identifying disposition and treatment plan.