Background: One of the challenges in hospital medicine is the care of patients overnight, when the primary team is unavailable, and care is being provided by those who are not as familiar with the patient. This is compounded by the high volume of pages at night. At UNC Rex Hospital, these factors resulted in delays responding to time sensitive issues.
Purpose: To decrease the hospitalist response time at night and improve nurse satisfaction by developing a more efficient communication method.
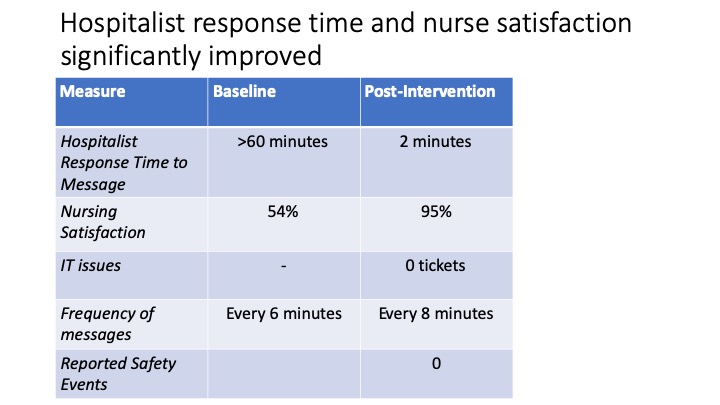
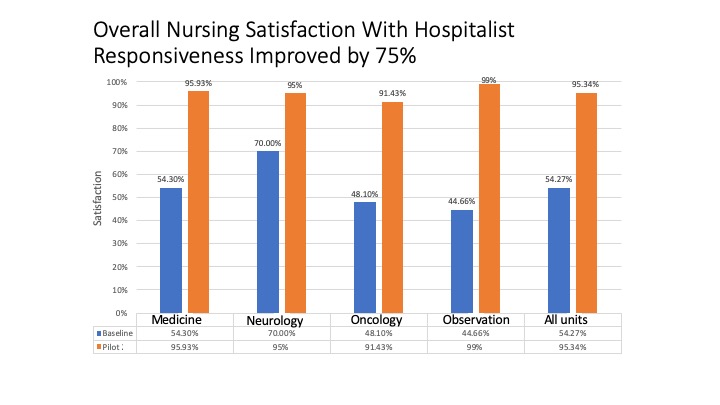
Description: The hospitalist team recorded all cross-cover messages over 14-night shifts. Each message was categorized as a clinical concern, new patient consult/admission, medication request, notification of abnormal test result or unnecessary. It was noted that the hospitalists received >100 messages in a 12-hour night shift. These messages occurred on average every 6 minutes and were not separated by class or priority. As a result, the hospitalists would respond to messages in the order received and not by acuity. This led to delays in responsiveness to time sensitive issues. The hospitalist team then collaborated with telecommunications and information technology (IT) to create a personalized build in the Vocera communications platform that allowed HIPAA compliant text messages to be identified by category and acuity. Nurses from four units (general medicine, oncology, neurology and observation) were asked to securely text through this platform at night. Nurses were trained on how to categorize texts as a clinical concern, new patient consult/admission, medication request or notification of abnormal test result. Nurses were also asked to classify texts as urgent, high or routine priority. Education was provided in the form of online modules and tip sheets. Nurse satisfaction with hospitalist response time was measured pre and post intervention. Response time was measured from the time a text was received to the time a response was sent. IT problems and safety events were also tracked. Hospitalist response time significantly decreased from over one hour at baseline to two minutes, while overall nurse satisfaction increased from 54% to 95%. There were no IT issues and no documented safety events related to the intervention. (Figures 1 and 2)
Conclusions: This multidisciplinary collaboration and optimization of technology reduced delays in patient care and improved nursing satisfaction. Based on this success, the process was expanded hospital wide and is now the standard for hospitalist-nurse communication at night.