Background: Peripherally inserted central catheters (PICCs) are one of the most widely used means for long term vascular access. When compared to traditional central venous catheters (CVCs), PICCs offer several advantages including safer insertion in the arm, cost-effectiveness, and easier self-care for patients outside the hospital. Despite these advantages, numerous studies have found complications associated with PICC placement including venous thromboembolism and central line-associated bloodstream infection. Studies suggest that an increasing number of lumens is associated with an increased risk of thromboembolism. A review of the literature suggests a large variation in the selection of single versus multi-lumen PICC placement in hospitalized patients.
Purpose: Our project aims to decrease the number of inappropriate multi-lumen PICCs through the implementation of a standardized consult pathway for vascular access and provider education.
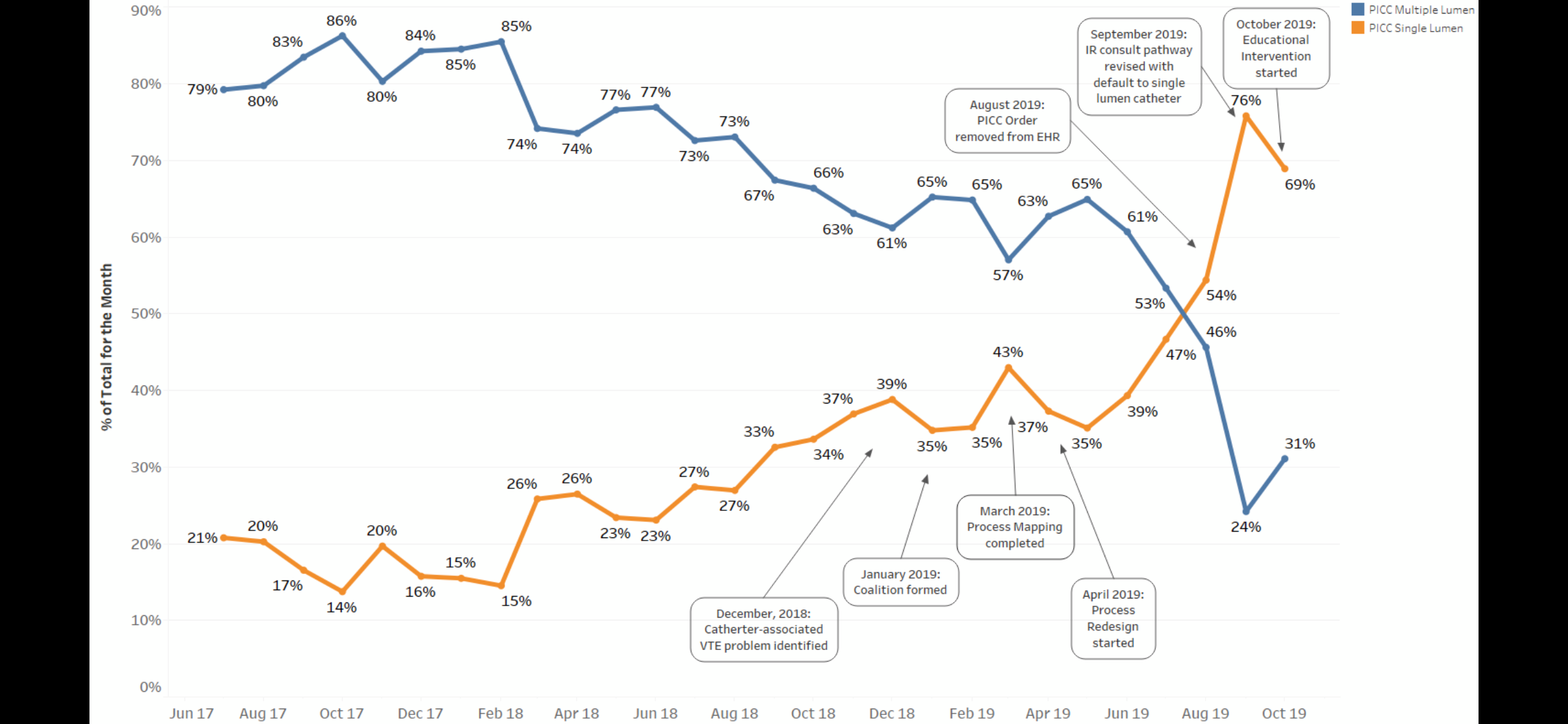
Description: This multifaceted, interdisciplinary study took place at a large, tertiary-care academic medical center between December 2018 and October 2019. The total number of PICCs placed was tracked from June 2017 to October 2019 and further classified based on the number of lumens. Interventions to decrease the number of inappropriate multi-lumen catheters were introduced in a stepwise approach between August and October 2019. First, a new ordering pathway was introduced to improve clinical workflow through the electronic health record (EHR) by automatically consulting Interventional Radiology to aid in selecting appropriate access. The default order in the pathway was also updated and changed to a single lumen catheter. Secondly, ordering providers, including housestaff, hospitalists, and general medicine attendings, were educated on appropriate PICC line practices using the Michigan Appropriateness Guide for Intravenous Catheters (MAGIC) through either in-person didactics or electronic mail. Following the intervention, the total number of single-lumen versus multi-lumen PICCs placed were compared.3484 PICCs were placed from June 2017 and October 2019. Prior to the intervention, 34.15% of all PICC lines placed were single lumen while the remaining 65.85% were multi-lumen catheters. After the order was updated in the EHR and defaulted to a single lumen PICC, 59.00% of PICC lines placed were single lumen catheters while the remaining 41.00% were multi-lumen.
Conclusions: Our study demonstrates the success of a stepwise, multi-faceted approach to decreasing the percentage of inappropriately placed multi-lumen PICCs compared to single lumen PICCs for hospitalized patients requiring long-term vascular access. A longer follow-up period is required to determine the impact of these updated practices on the incidence of venous thromboembolism and central-line associated bloodstream infections in patients requiring PICCs. As hospitals continue to meet demands to demonstrate meaningful use of the EHR, we propose ongoing efforts to optimize order sets as well as enhance physician education and patient safety.