Background: Intravenous (IV) low molecular weight iron dextran is a safe and effective treatment for iron deficiency anemia (1). However, oral (PO) iron supplementation remains a preferred mode of iron repletion due to low cost and ease of administration. Unfortunately, the efficacy of PO iron varies due to differences in drug absorption and patient adherence. Treatment with PO iron also takes longer than treatment with IV iron. This becomes especially important in the preoperative setting where patients often present for preoperative evaluation within weeks of an upcoming surgery. Prior studies have shown that IV iron is effective at reducing requirement for packed red blood cell (PRBC) transfusion when combined with an erythrocyte stimulating agent (ESA) (2). This study examines the efficacy of IV iron treatment without ESA versus PO iron treatment in the perioperative period.
Methods: We performed a retrospective study of patients with iron deficiency anemia undergoing surgery between 2014 and 2019. Iron deficiency anemia was defined as hemoglobin less than 13 g/dL in males or 12 g/dL in females, with an accompanying iron saturation less than 15 ng/mL. These patients were divided into two categories based on the type of iron they received – IV versus PO. Patients with pregnancy and end stage renal disease were excluded. Demographic data, pretreatment laboratory values, preoperative laboratory values, and the type of surgery were recorded. Surgeries were ranked as intermediate, high, and very high risk based on a Preoperative Risk Stratification Tool (3). Surgeries that were less than intermediate risk were excluded. The number of PRBC transfusions given between surgery and hospital discharge were recorded. Two sample T-tests were run for means and Fisher’s exact test was used for categorical variables. Results were considered significant for a p value < 0.05.
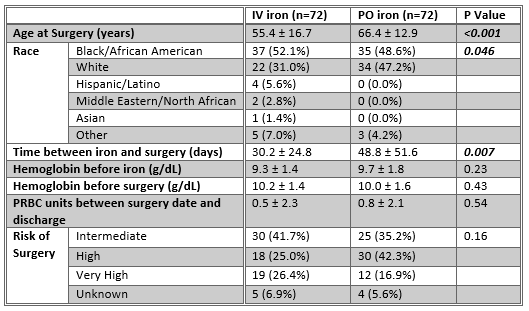
Results: A total of 144 patients were included in this study, 72 who were treated with IV iron and 72 who were treated with PO iron. Our population was predominantly African American (50.3%), followed by Caucasian (39.2%). There was no significant difference in pretreatment hemoglobin, preoperative hemoglobin (within 24 hours prior to surgery), gender, or surgical risk. However, there was a significant difference in age between the two groups – the PO iron group was, on average, about 10 years older than the IV iron group (66.4 ± 12.9 years vs 55.4 ± 16.7 years, p = <0.001). There was also a significant difference in terms of race; African American patients were more likely to receive IV iron than Caucasian patients (p = 0.046). There was a trend toward longer treatment periods for PO iron than IV iron (48.8 ± 51.6 days vs 30.2 ± 24.8 days, p = 0.007). While not a statistically significant difference, the average hemoglobin increase in the PO iron group was 0.3 g/dL, while the increase in the IV iron group was 0.8 g/dL. After surgery, there was no significant difference in the number of packed red blood cell transfusions (PRBCs) given prior to hospital discharge.
Conclusions: There was no significant difference in preoperative hemoglobin or postoperative PRBC transfusion between the PO iron and IV iron treatment groups. However, the two groups did differ in three key ways. First, the IV iron group was significantly younger. Second, the IV iron group was generally treated closer to the date of surgery. And third, the patients receiving IV iron were more likely to be African American. The differences in prescribing patterns between ages and races merit further investigation.