Background: Evaluating a patient’s post-hospitalization course is critical feedback for refining future diagnostic and therapeutic decisions, yet it rarely happens formally during residency. The Out of Sight, Out of Mind (OOSOOM, pronounced like “awesome”) conference addresses this gap.
Purpose: To provide a structured forum for residents to review post-discharge outcomes of the patients they managed and with coaching, share them with colleagues, focusing on lessons learned and changes they would implement in their practice as a result.
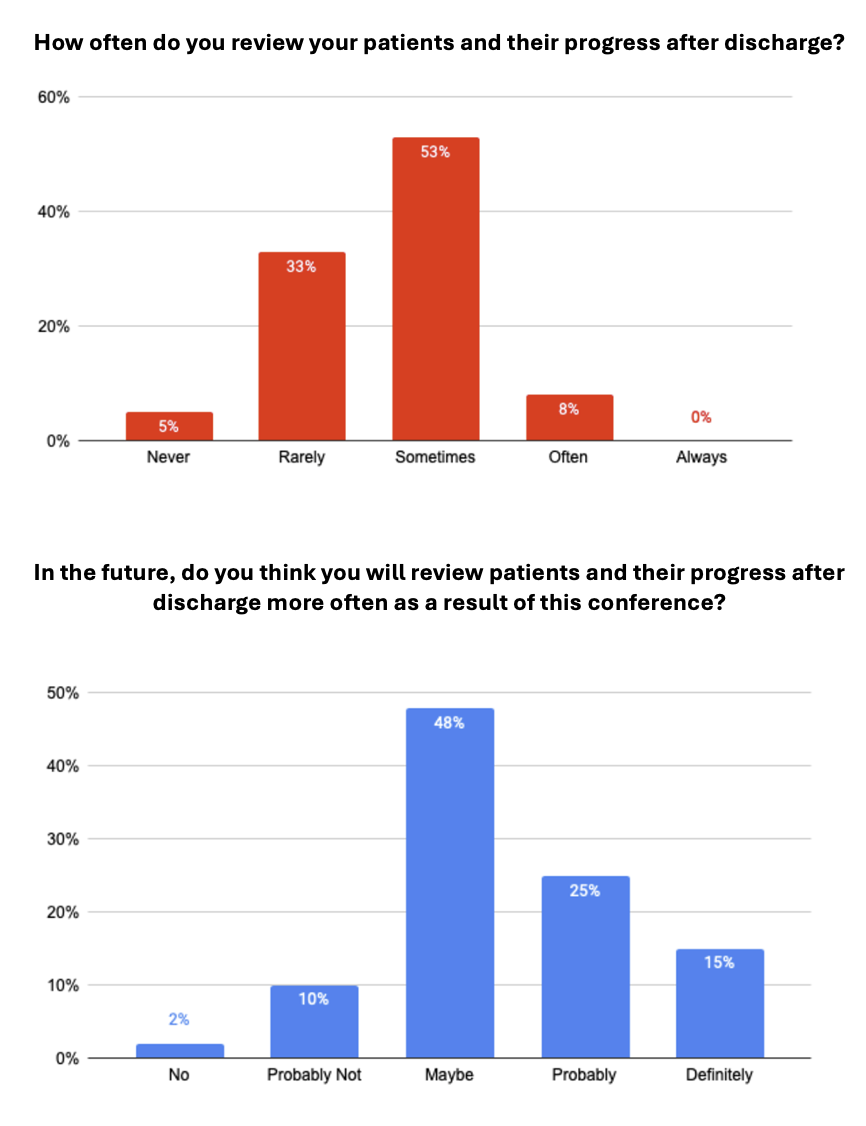
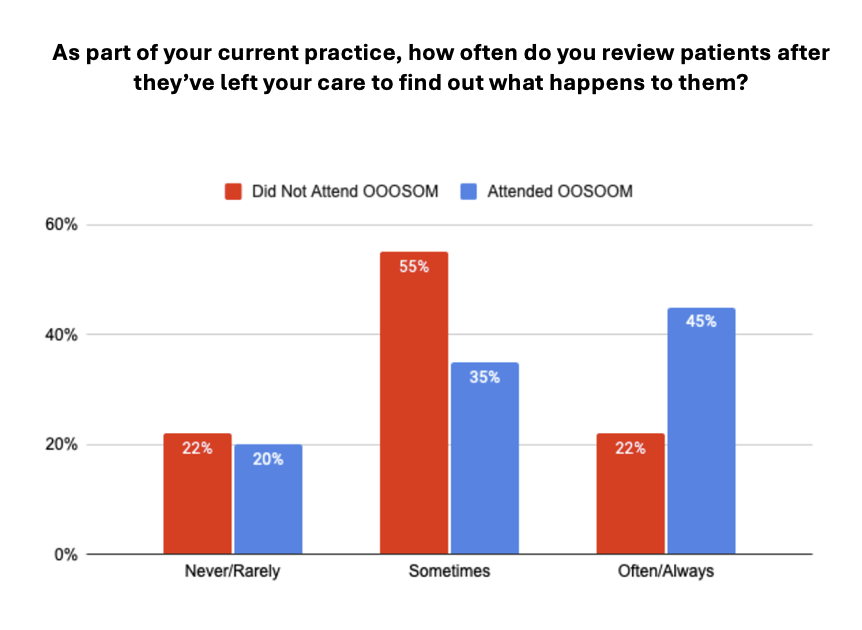
Description: We created an easy-to-implement, resident-led conference to review post-hospitalization outcomes. Residents are given lists of patients that they discharged in the previous six months and select one case to present at an OOSOOM conference. Four residents present their cases at each conference. Each presenter reviews five to ten patients who have post-hospitalization outcome data available in the EMR. We encourage them to gather additional information by calling patients. They are asked to pay special attention to patients whose post-hospitalization course differs from the team’s expectations at the time of discharge. Each resident creates a presentation using de-identified patient information, and we coach them to describe lessons they learned and changes they would make in their future practice. We studied the effect of OOSOOM by administering a retrospective pre/post survey immediately following the first four conferences and a follow-up outcome survey two to four years after participation in OOSOOM. Prior to OOSOOM, only 8% of residents reported reviewing their patients’ post-hospitalization progress “often” or “always.” After the conference, 41% of residents said they would “probably” or “definitely” review their patients’ outcomes. In the follow-up outcome survey, of the residents who had attended at least one OOSOOM conference during residency, 45% reported reviewing patients after they leave their care “often” or “always” as part of their current practice compared to 22% of residents who had not attended an OOSOOM conference. These results suggest that there may be practice-changing value in such conferences.The format of OOSOOM achieves the dual goals of giving residents an opportunity to reflect on their practice and cultivating the habit of auditing post-hospitalization outcomes. OOSOOM also identifies opportunities for quality improvement projects and builds medical knowledge via experiential learning. Unlike a traditional Morbidity & Mortality (M&M) conference, in OOSOOM, residents are not limited to presenting negative outcomes and cases where care was suboptimal. Many choose to focus on diagnostic feedback, resulting in discussions more conducive to learning. In addition, unlike a traditional M&M, the outcomes residents discuss are often only uncovered by their review of post-hospitalization records rather than being reported in a quality or mortality review. Having this freedom allows residents to direct their own learning and influence their colleagues, thus advancing the overall goal of inspiring lifelong learning.
Conclusions: OOSOOM creates a system for post-hospitalization outcome review, reflection, and dissemination of findings. The results from the follow-up outcome survey are encouraging and suggest that there may be practice-changing value in such conferences.