Background: Hip fractures are a major health problem in the geriatric population in the United States, with estimated costs of $18B annually. Hip fractures are highly morbid in the elderly, as deconditioning and acute complications compound chronic comorbidities. To improve care for this high-risk population, hip fracture patients are preferentially admitted to our medicine hospitalist service with co-management from the orthopedics consult service. However, due to a variety of logistical factors (e.g., bed availability), some hip fracture patients are admitted to non-hospitalist services (e.g., orthopedics). The purpose of our study is to compare outcomes for hip fracture patients on hospitalist vs. non-hospitalist services.
Methods: We included all discharges from UNC Hospitals from July 2014 – June 2015 with a primary ICD-9 diagnosis of hip fracture. We excluded patients if they were ≤18 years old, if the hip fracture was caused by “high energy” trauma (e.g., motor vehicle accident), or if patients did not have an operative procedure. Logistic regression was used to examine patient demographic and clinical factors associated with length of hospitalization (LOS) ≤ 7 days and 30-day readmission. All covariates associated with ED revisits and 30-day readmission at the p-value ≤ 0.25 level in the univariate analyses were included in the adjusted model.
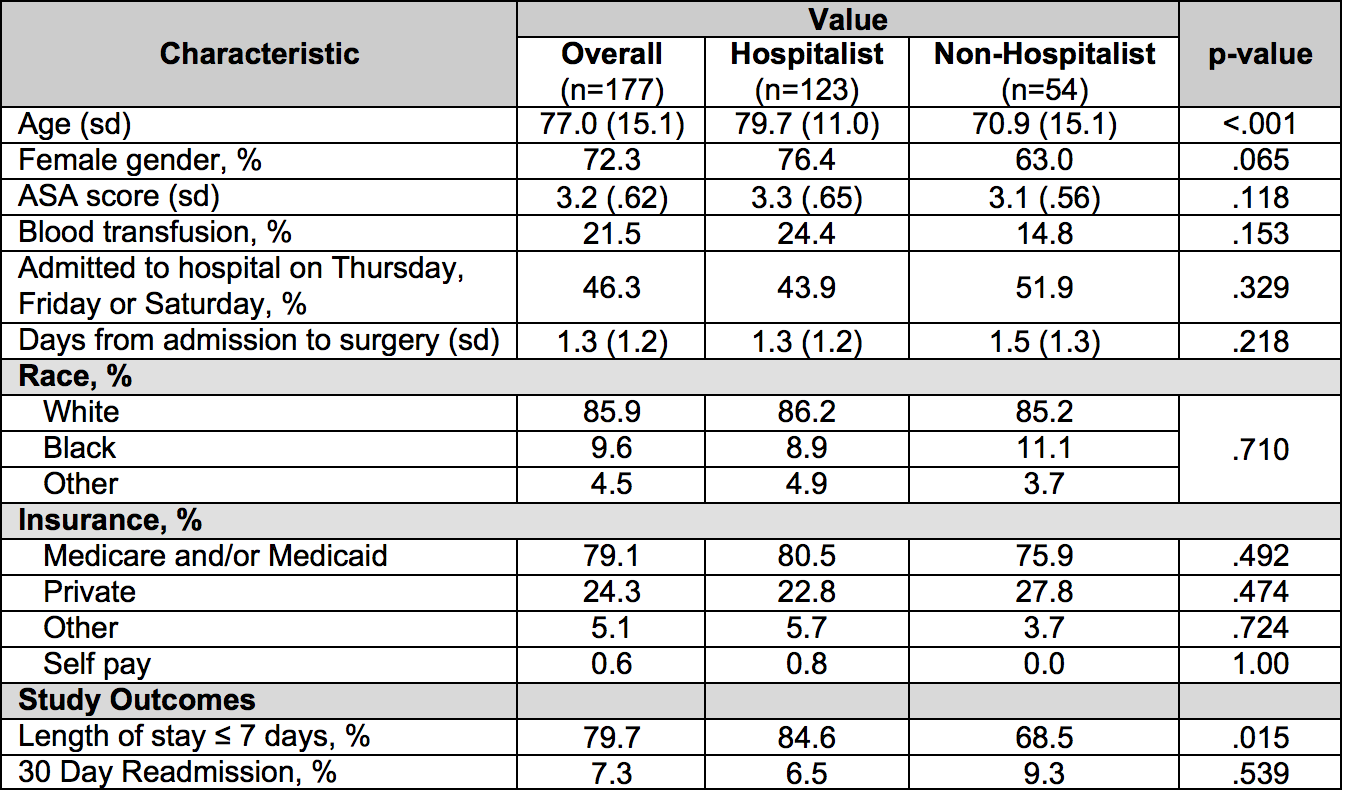
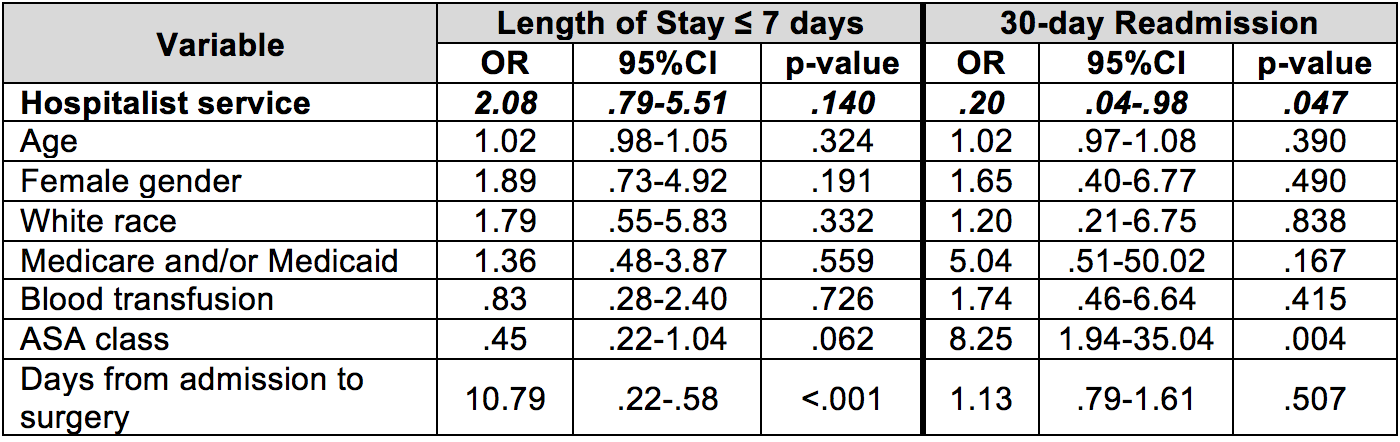
Results: 177 patients were included in the study (123 on hospitalist and 54 on non-hospitalist services) (table 1). In adjusted analyses (adjusting for demographics, disease severity using the American Society of Anesthesia (ASA) score, administered blood transfusion, days from admission to surgical procedure), patients on the hospitalist service had reduced 30-day readmission rates (OR: 0.2, p-value=0.047) and a trend toward reduced length of stay (OR: 2.08, p-value=0.140) (table 2).
Conclusions: In our study, patients with hip fracture admitted to a hospitalist versus a non-hospitalist service had significantly reduced 30-day readmission rates and a trend towards reduced length of stay. Future studies will investigate which care processes on the hospitalist service are associated with improved patient outcomes.