Background: Assessing and treating pain in older adults is challenging. Although having patients self-report pain on a numeric scale is the recommended approach, age-associated conditions such as dementia, delirium, and impaired vision or hearing can prevent patients from effectively communicating their symptoms. Older patients are also at risk of adverse effects from commonly used analgesics such as opioids, making clinicians more cautious. Yet little has been published about how pain is assessed and recorded in older adults and whether geriatric-related conditions are associated with diagnosis and treatment.
Methods: We conducted a retrospective analysis of all adults 65+ years who were hospitalized on the acute general medicine service at a large urban teaching hospital, over an ~8-year period from 2013-2021. Standard nursing documentation includes regular assessment of pain, which is divided into self-reported tools, including the Numeric Rating Scale, and behavioral assessments. All pain documentation was from nursing flowsheets, including the numeric pain score if performed. Patient-level demographic and medical factors were from electronic health records, including diagnosis codes for dementia or mild cognitive impairment (MCI), visual or hearing impairment, whether a geriatric consult was performed, and end-of-life care. Medication administration records provided the average daily morphine milligram equivalent (MME) received.We first described how frequently specific pain assessment tools were used in this older population. Next, we examined whether patient-level factors were associated with how pain was assessed, with specific focus on the numeric rating scale. Then, among patients with numeric pain scores, we determined whether average numeric scores were associated with specific age-related variables and average daily MME, adjusted for patient level factors.
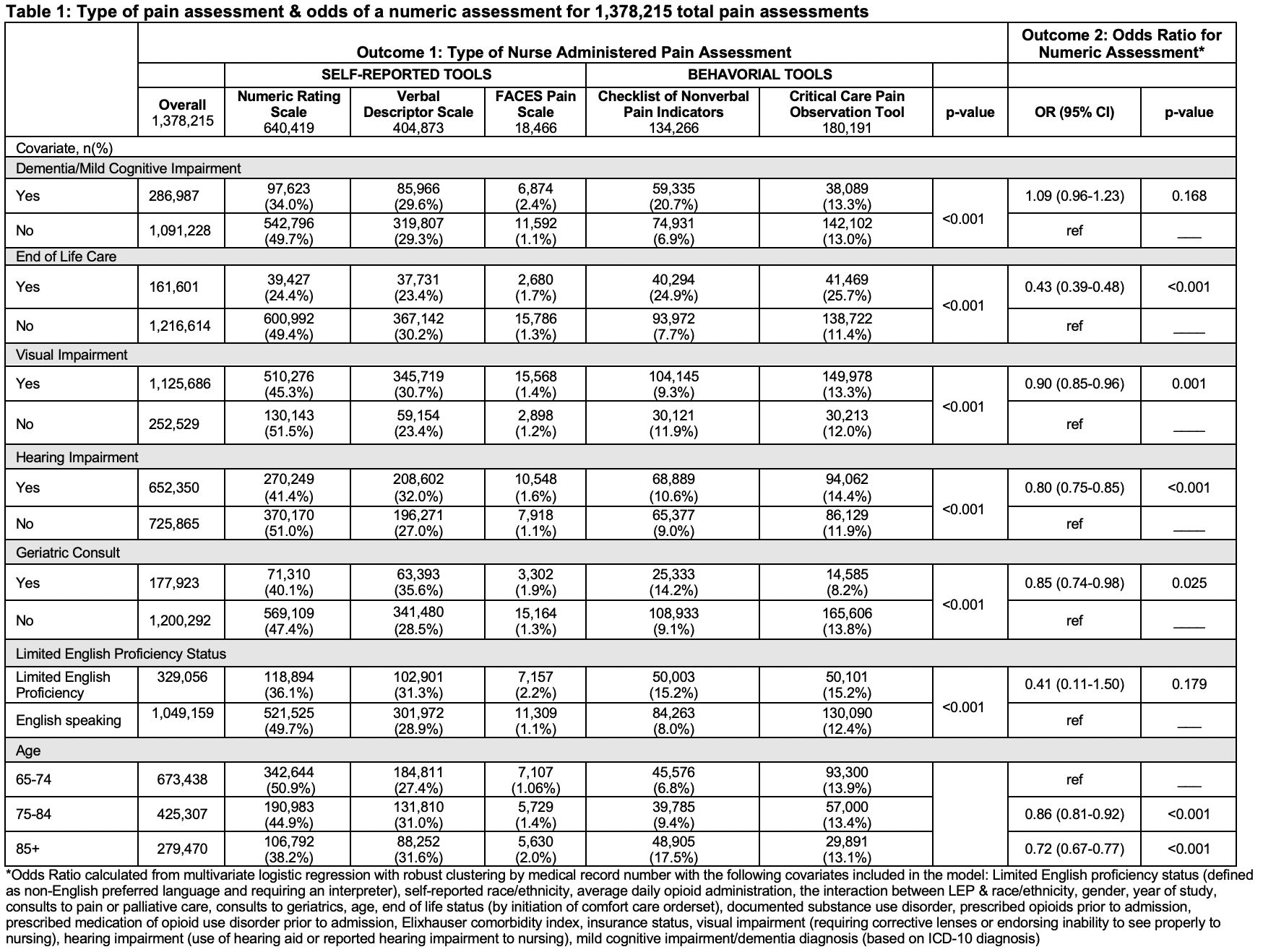
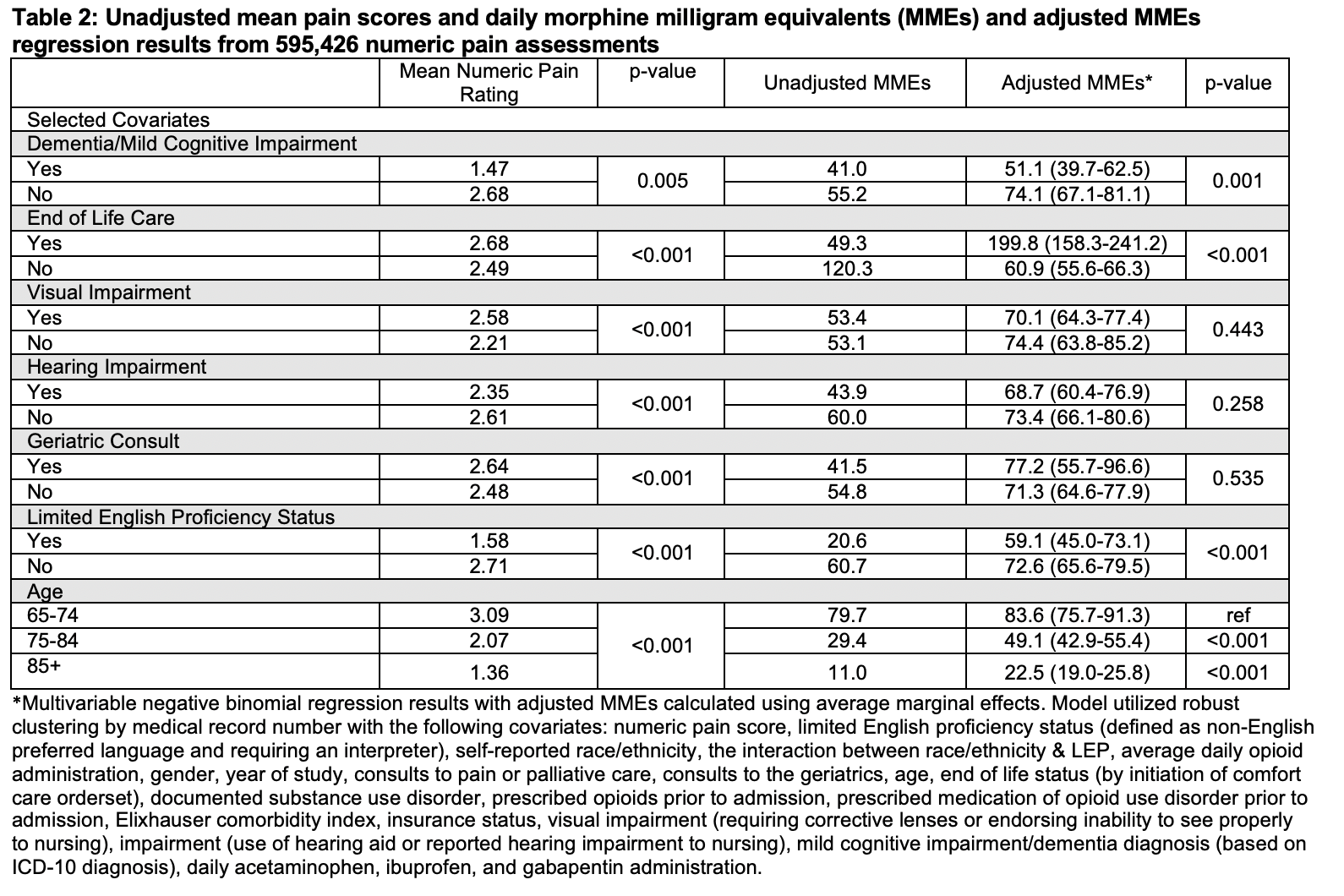
Results: Our cohort included 27,857 hospitalizations and 1,378,215 pain assessments. 77% of assessments used self-report tools, most commonly the numeric rating score. However, the type of pain assessment tools used varied by patient factors (Table 1). Visual impairment (OR 0.90, 95% CI 0.85-0.96), hearing impairment (OR 0.80, 95% CI 0.75-0.85), end-of-life care (OR 0.43, 95% CI 0.39-0.48), geriatrics consult (OR 0.85, 95% CI 0.74-0.98), age between 75-84 (OR 0.86, 95% CI 0.81-0.92), and age 85+ (OR 0.72, 95% CI 0.67-0.77) were all associated with lower odds of having pain recorded using numeric assessments. Among the 26,641 patients who had numeric pain scores, older age was associated with lower average numeric pain scores (Table 2). After multivariable adjustment, compared to patients aged 65-74, patients aged 75-84 (-34, 95% CI -43 – -26) and patients older than 85 (-61, 95% CI -68 – -54) received fewer opioids. Dementia/MCI (-23, 95% CI -35 – -11) and limited English proficiency (-13.5, 95% CI -27 – -0.5) were associated with a lower average MME and end-of-life care was associated with higher average MME (139, 95% CI 98-179).
Conclusions: Numeric pain scores, which are widely recommended and used to guide treatment of pain, are less likely to be used in older patients and those with hearing and visual impairment, geriatrics involvement, or at the end-of-life. Older age, a diagnosis of dementia/MCI, and limited English proficiency were associated with lower average opioid administration, even after controlling for other factors. These findings identify a group of patients for which pain may be underreported and undertreated.