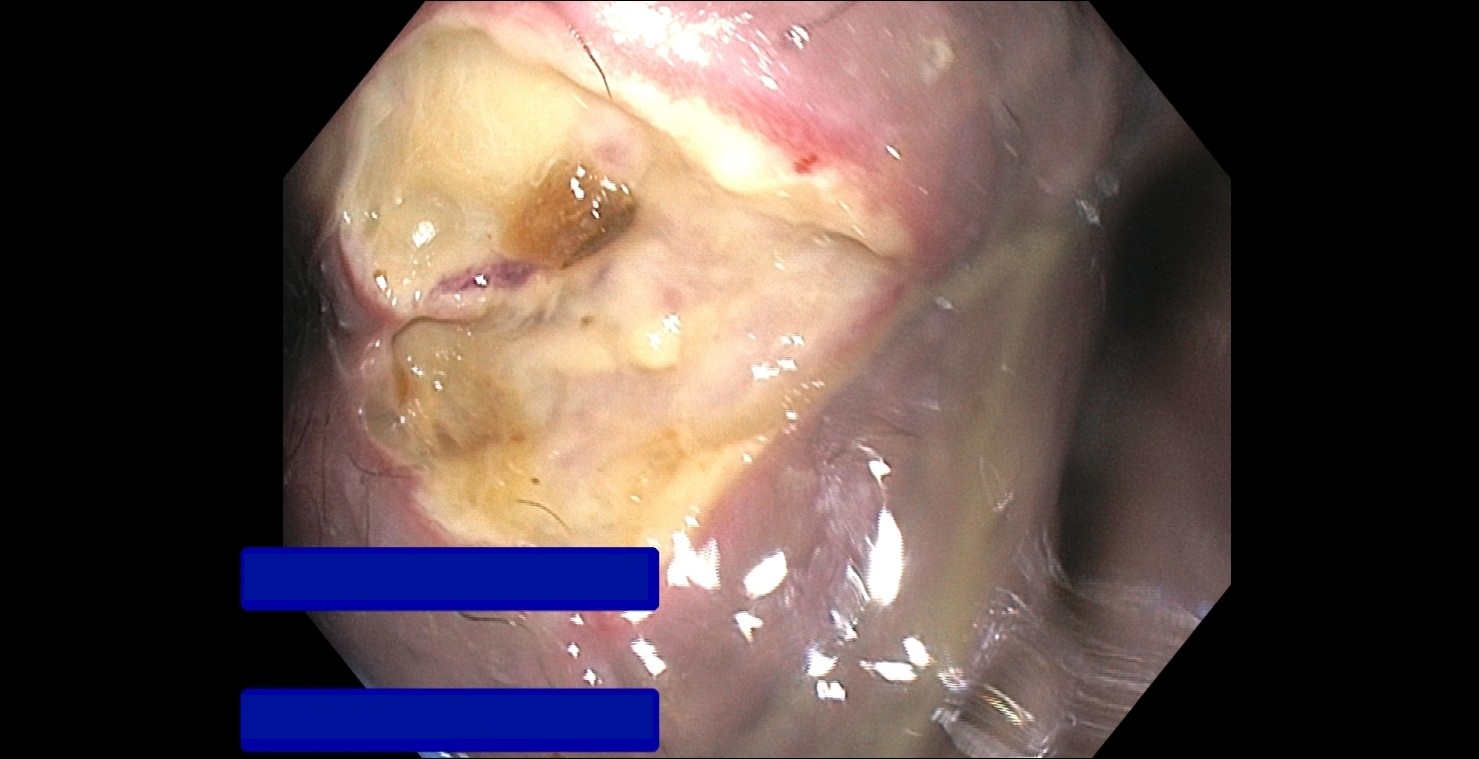
Case Presentation: A 27-year-old male with end stage renal disease from focal segmental glomerulosclerosis with living donor transplant and progression to chronic kidney disease presented with 2 weeks of diarrhea, proctalgia, and hematochezia. On presentation he was afebrile and hemodynamically stable. Rectal exam showed significant tenderness, no hemorrhoids or fluctuance, and mucous-like drainage. Labs showed white blood cell count 2,400 µl, hemoglobin 12.8 g/dL, and creatinine 1.89 mg/dL. Computed tomography of the abdomen and pelvis showed mild rectal wall thickening and perirectal and anal fat stranding compatible with proctitis without abscess.He was started on ciprofloxacin and metronidazole for suspected proctitis, though he developed worsening bowel incontinence and diarrhea. Repeat rectal exam showed a large anal fissure. Antimicrobials were escalated to piperacillin-tazobactam, linezolid, and micafungin. He underwent flexible sigmoidoscopy which showed an 8 x 7 cm ulcer abutting the anal canal (Figure 1, 2) with a normal rectum, sigmoid, and descending colon. Ulcer brushings were negative for adenovirus, monkeypox, herpes simplex virus (HSV)-1 and -2, and cytomegalovirus (CMV). Anorectal exam under anesthesia showed a perianal fistula connecting the anal ulcer and fissure, which were treated with ulcer debridement, fistulotomy, and botulinum toxin injection.His infectious workup of the serum included a negative CMV polymerase chain reaction (PCR), Epstein-Barr virus (EBV) PCR, HSV-1 and -2 PCR, varicella zoster virus PCR, and rapid plasma reagin. Further negative testing included a negative urine and rectal Nisseria gonorrhoeae and Chlamydia trachomatis PCR, Histoplasma capsulatum urine antigen, Clostridioides difficile toxin, gastrointestinal molecular pathogen panel, anal methicillin-resistant Staphylococcus aureus PCR, and fecal calprotectin. He had a positive stool acid fast bacillus (AFB) culture, though ulcer swab was negative for AFB. His final diagnosis was an infected perianal ulcer complicated by fissure and fistula. He was discharged with doxycycline and amoxicillin clavulanate for a total of 14 days for cellulitis of the ulcer due to Mycoplasma genitalium versus Staphylococcus aureus.
Discussion: An anal ulcer is an open sore with loss of mucosal surface and necrosis of the tissue. Diagnosis includes exam under anesthesia with biopsies and cultures. The etiology of anal ulcers includes CMV, HSV, human immunodeficiency virus (HIV), syphilis, Chlamydia trachomatis, tuberculosis, malignancy, and idopathic1,2. They are slow to heal and treatment frequently requires antimicrobials. Anal ulcers represent 10-15% of anal pathology in immunocompromised patients2. An anal fissure is a cleft or groove which causes rectal pain and bleeding. They can often occur due to constipation, diarrhea, vaginal delivery, and anal trauma. Seventy-five percent of anal fissures have a posterior midline location3,4,5. Less than 1% of fissures are off midline and these are atypical fissures that require further evaluation with biopsies and cultures. The etiology of atypical fissures includes Crohn’s disease, anal cancer, syphilis, herpes, CMV, HIV, human papilloma virus, tuberculosis, and histoplasmosis3,4.
Conclusions: Hospitalists should have a high degree of suspicion for diagnosis of anal ulcers and atypical anal fissures, especially in immunocompromised patients.