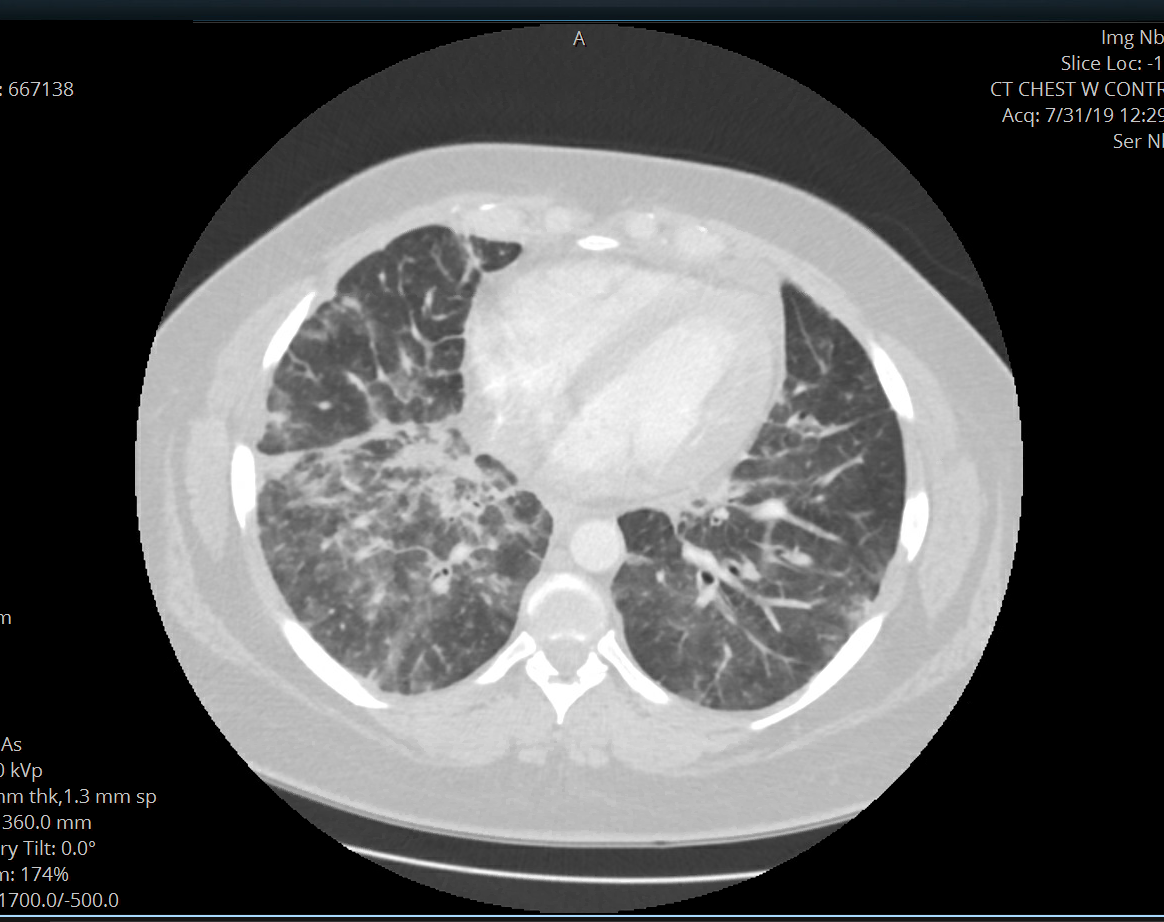
Case Presentation: A 35 year old African American woman with a past medical history of alcohol and tobacco abuse and acute pancreatitis presented to the hospital with a progressive dyspnea and nonproductive cough for one month not responding to outpatient antibiotics. Six months prior to presentation, she was hospitalized for acute pancreatitis that was attributed to her binge drinking. Patient denied any fevers, orthopnea, or lower extremity edema. Patient was afebrile on admission with normal white blood cell count. Computed tomography (CT) of the chest showed diffuse ground-glass and consolidative opacities (most pronounced in perilymphatic distribution). Broad spectrum antibiotics were started empirically however given low suspicion for an infectious process, patient was referred for a lung biopsy. Inflammatory pneumonitis and Interstitial lung disease, due to connective tissue disease, vasculitis, or idiopathic, were part of the differential diagnosis. Antinuclear antibodies (ANA), rheumatoid factor (RF), complements C3 and C4, antineutrophil cytoplasmic antibodies (ANCA) all returned normal or negative. Patient underwent video-assisted thoracoscopic (VATS) biopsy. Pathology was consistent with metastatic adenocarcinoma, lymphangitic pattern, with morphologic features and immunoprofile suggestive of an upper gastrointestinal or pancreaticobiliary primary. CT of abdomen and pelvis revealed a pancreatic mass. Patient was discharged and underwent her first cycle of chemotherapy treatment with leucovorin, fluorouracil, irinotecan, and oxaliplatin (FOLFIRINOX). Five days later, patient was readmitted with respiratory failure and was found to have acute segmental pulmonary embolism and worsening metastatic lung disease. Despite treatment with therapeutic heparin, her pulmonary status further declined. She transitioned to hospice care six weeks after her initial diagnosis of metastatic pancreatic cancer.
Discussion: There are no screening recommendations for pancreatic cancer in the United States. Acute pancreatitis is rarely the presenting symptom; but even more rare is pulmonary symptoms from lymphangitic spread. In retrospect, there was an opportunity to diagnose pancreatic cancer much earlier in this patient when she presented with acute pancreatitis, however, further testing was not indicated in this patient, given her young age, presence of a common risk factor for acute pancreatitis, and lack of other alarming symptoms. Imaging obtained at the time of her diagnosis of acute pancreatitis showed a 13 mm pancreatic mass versus developing necrotizing pancreatitis and early pseudocyst, however, patient was lost to short-term follow up.
Conclusions: This was an unusual presentation of pancreatic cancer in a young woman admitted with pulmonary symptoms from lymphangitic carcinomatosis. In patients presenting with dyspnea and cough without any signs of infection and no response to the standard antibiotic therapy for bacterial pneumonia, alternate diagnoses should be considered. When the diagnosis is unclear, a referral for lung biopsy can be helpful in arriving at the diagnosis.