Background: A frequently cited challenge to parenting as a clinician relates to family leave policies. Taking parental leave may negatively affect clinicians’ income, research, career, and relationships with colleagues. Parental leave policies may be unfair, vague, or poorly communicated. We sought to describe the parental leave experiences and approaches used to support parental leave and return in hospital medicine.
Methods: The Hospital Medicine Reengineering Network [HOMERuN] collaborative engages hospitalists across the nation to support research and dissemination of strategies to improve hospital medicine. We conducted virtual, semi-structured focus groups through the HOMERuN network. Questions focused on parental leave experiences. We utilized rapid qualitative methods including templated summaries and matrix analysis to identify themes from the data
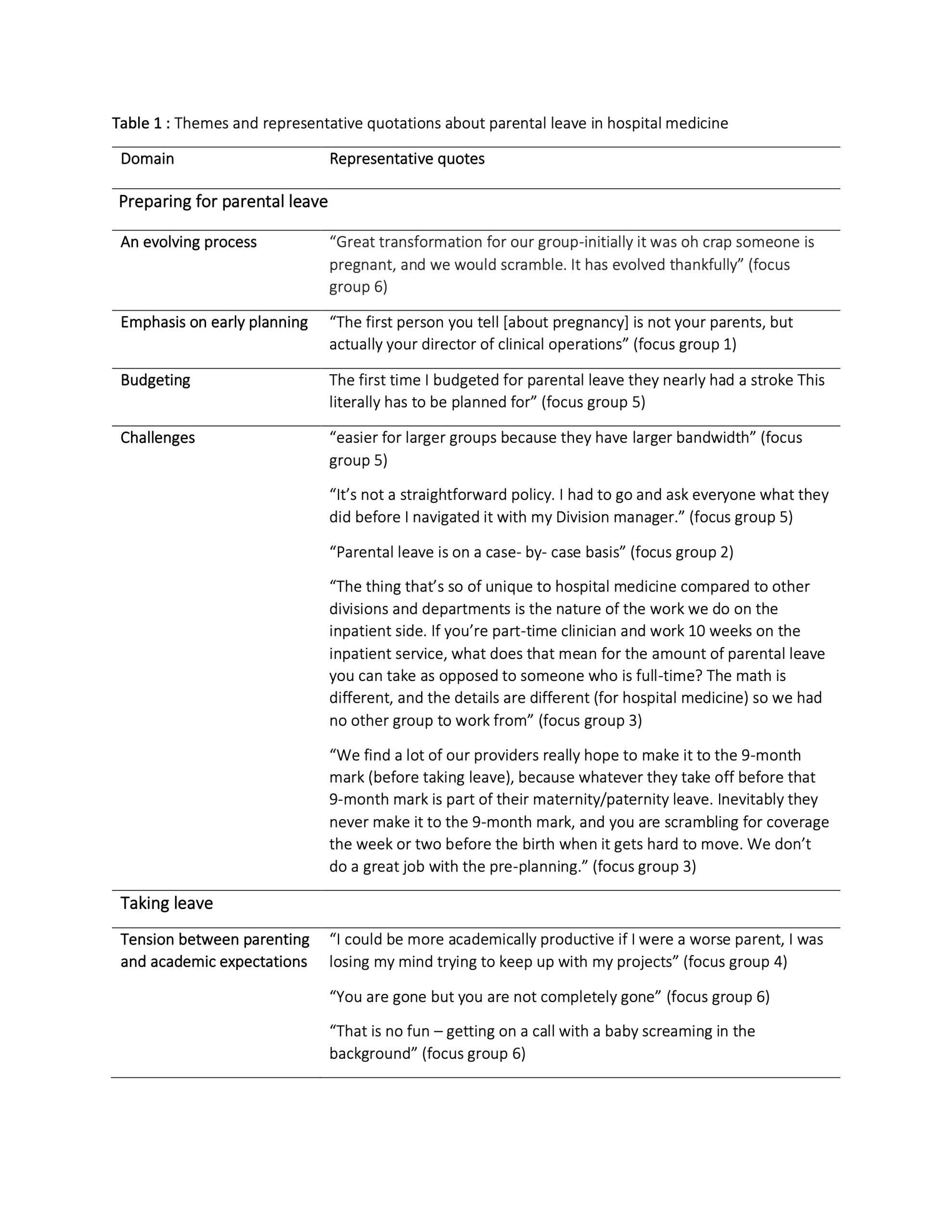
Results: There were 21 participants from 15 unique sites, 13 (61%) were women and 19 (90%) had leadership positions.Emerging themes were categorized into four domains: how institutions and hospitalists prepare for parental leave, the experience of taking leave, the experiences upon return and how we can improve. (Table 1)PreparingParental leave was described as ‘evolving’ at many sites- with more sites recently offering leave for all parents. An emphasis on better planning was noted- both by staffing to anticipated needs and by fostering a culture that encourages earlier disclosure of pregnancy. Challenges included support for budgeting and staffing designed to anticipate parental leave, the complexity of hospitalists’ work affiliations and the lack of familiarity with hospitalist specific circumstances by colleagues in human resources. Hospitalists described the need to advocate for themselves in the face of complex, opaque policies. Often hospitalists continue to work until delivery.Taking leaveParental leave itself was described as ‘disappointing’ with immense variation in parental leave policies across sites including duration and eligibility. Many described continuing to work in their non-clinical roles during leave and expressed concerns about the hand-off of their administrative and research roles as they juggled parenting and academic expectations. A shift in the culture over the last several years with decreased resiliency by those covering for colleagues on leave was noted.ReturningUpon return, support systems were often focused on supporting lactation. Some health systems provide lactation credits and census reductions for lactating women. Childcare following birth was described as increasingly challenging. The lack of support was felt to disproportionately impact women, with women often reducing or altering their roles.The way forwardAs participants envisioned a way forward, the role of how our culture values parenting and shapes expectations emerged. The contrast between policies in the US versus other countries was apparent. Improving support for the workday of a hospitalist by using discharge RNs, safe workloads etc. was also identified as a powerful tool to support hospitalists at all stages of their life-cycle.
Conclusions: Parental leave in hospital medicine poses unique challenges. These challenges are consequential and may disproportionately impact women in hospital medicine. Concerted, multifaceted efforts to address our policies, procedures, staffing, culture and expectations that span preparing, taking and returning from parental leave are needed.