Background: Sound Hospital Medicine (HM) and Sound Emergency Medicine (EM) staff a 385-bed hospital in California. The Utilization Review (UR) nurses in the ER were not following the hospital’s Utilization Management (UM) Plan of doing initial InterQual reviews before the hospitalist wrote the initial admission order because of the focus on disposition from the ER. Conditions of Participation (CoP) require that hospitals screen for medical necessity. There was a lack of alignment. The hospital had a centralized UR team that did day 1 InterQual reviews after admission. The initial admission status that the hospitalist assigned the patient often did not match the day 1 InterQual review. This resulted in excessive UR and hospital physician advisor (PA) resources. The hospital had a high number of denials. In the other hospitals in the system where admission status was assigned based on initial InterQual review level of care, the denials were much lower.
Purpose: Sound Advisory took over the InterQual initial status reviews so the UR nurses could keep doing the disposition work that they were doing. Sound Advisory provided education for the ER and HM providers on admission status and what was going on with denials. The HM provider entered the admission order based on the InterQual initial review, with consideration of the anticipated length of stay for the Medicare FFS patients. We implemented a process for our PAs to automatically review every Medicare FFS patient in observation status after 1 midnight if they were going to be staying a second midnight. As the hospital continued to have centralized UR nurses perform Day 1 InterQual reviews they maintained their compliance with CoP. The goal was to improve the alignment of admission status ordered with InterQual level of care criteria to decrease denials.
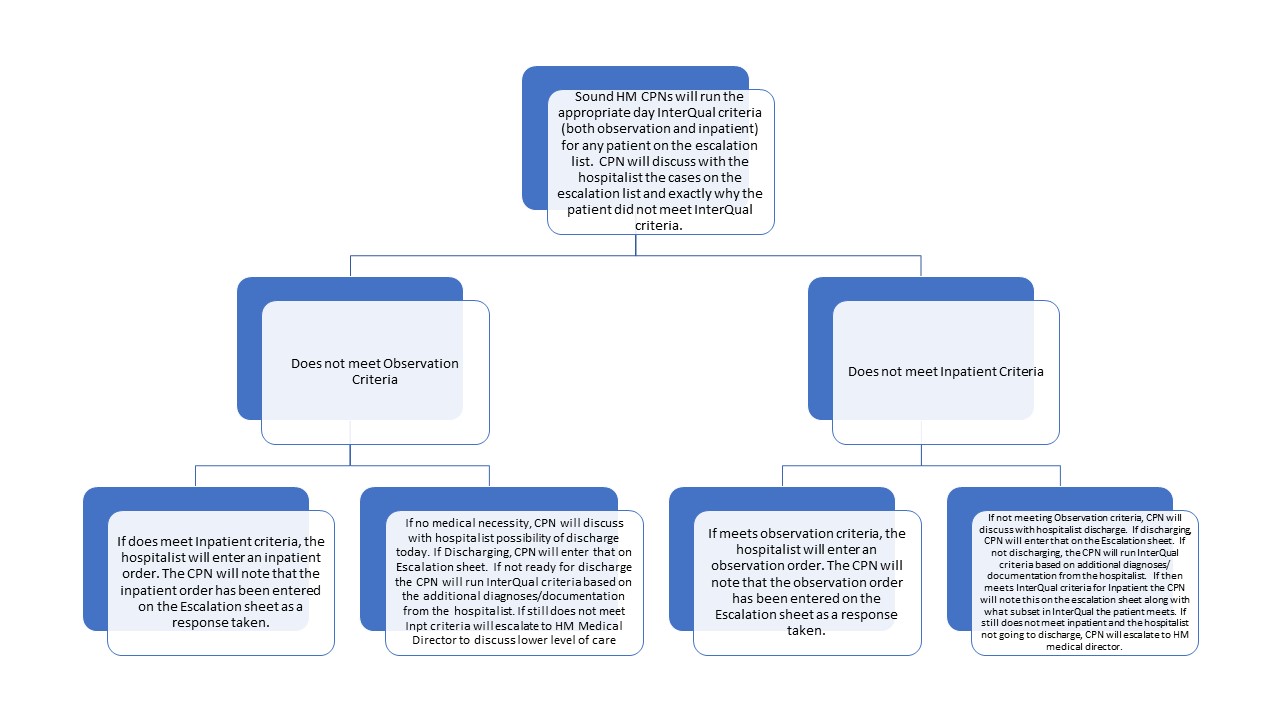
Description: Sound Advisory began with educating and staffing nurses to do remote InterQual Initial Reviews after making training videos and handouts on the process. The ER clerk sent a Tiger Text message to the hospitalist and Sound Advisory nurse with the name of the ER patient to be admitted. The hospitalist would write the admission order based on the InterQual Initial Review recommendation with the caveat for the Medicare FFS anticipated length of stay. Through the billing software for the hospitalists, we were able to automate a report for all Medicare FFS patients who were in observation status. After 1 midnight our nurses would screen to determine if the patient was staying a second midnight in the hospital. For these patients, the Sound PAs would review the EMR to determine if inpatient status was appropriate. If the patient was appropriate for inpatient level of care, the PA would communicate directly with the hospitalist and request the inpatient order.
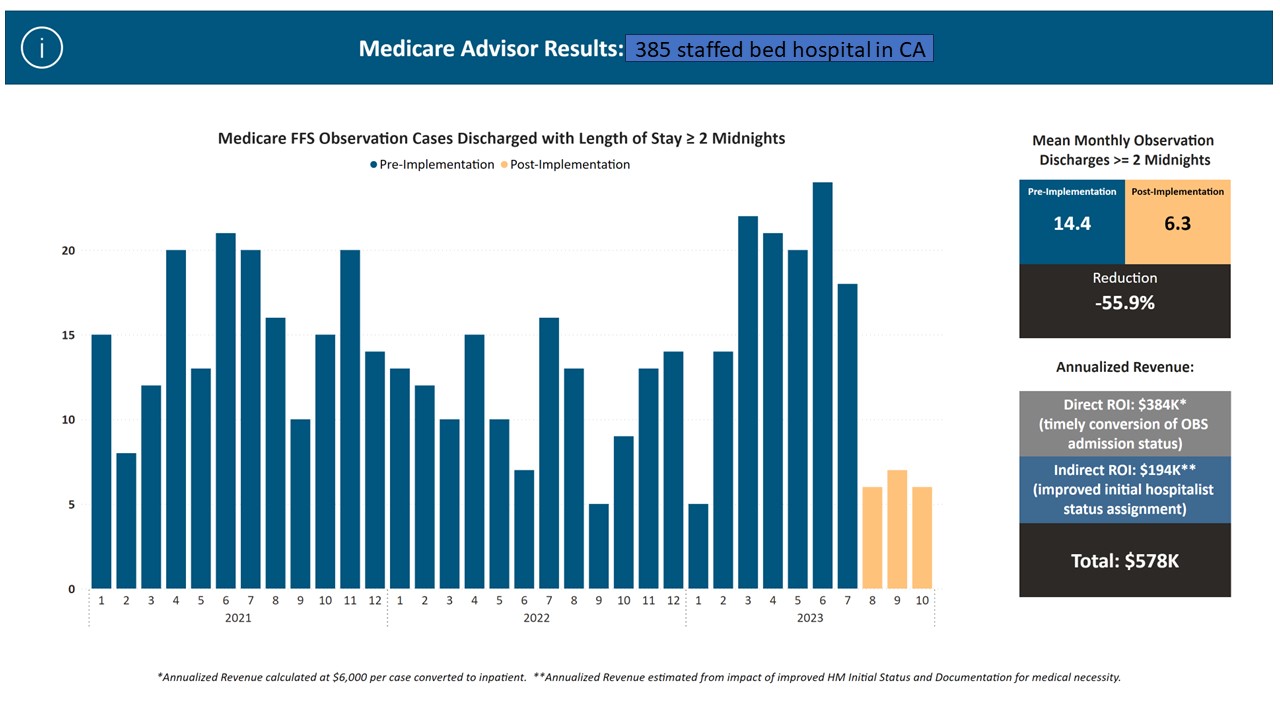
Conclusions: After Sound Advisory implemented the process, the number of patients not meeting day 1 InterQual level of care went down significantly. Sound Advisory tracked the number of patients who met for inpatient, observation, and no level of care. This process can be used for feedback for the ER and HM providers. This helps to ensure that no ER provider has excessive admissions for patients without medical necessity. The rate of Medicare 2-midnights or longer observation stays went from 14.4 per month to 6.3 per month. This results in an approximately $578,000 annual revenue increase for the hospital as the hospital is reimbursed approximately $2300 for an observation stay and the hospital is reimbursed approximately $8300 for the average medical DRG.