Background: An effective patient safety and quality improvement (QI) curriculum is imperative for graduate medical education (GME) training programs. Yet many health systems are lacking pedagogical training in these methods. Learning often takes the form of group project work, yet projects may not reflect institutional priorities, duplicate ongoing efforts, or remain unfinished after allotted time for group work is completed. As a result, residents feel their contributions to the broader missions of safety and quality within the institution are limited and of little value.
Purpose: The purpose of this innovative program was to develop a novel curricular method aligning Internal Medicine Residency Program (IMRP) patient safety and QI group project work with institutional goals. This was achieved by providing structured support from engineering experts to resident groups for optimal learning of safety and quality.
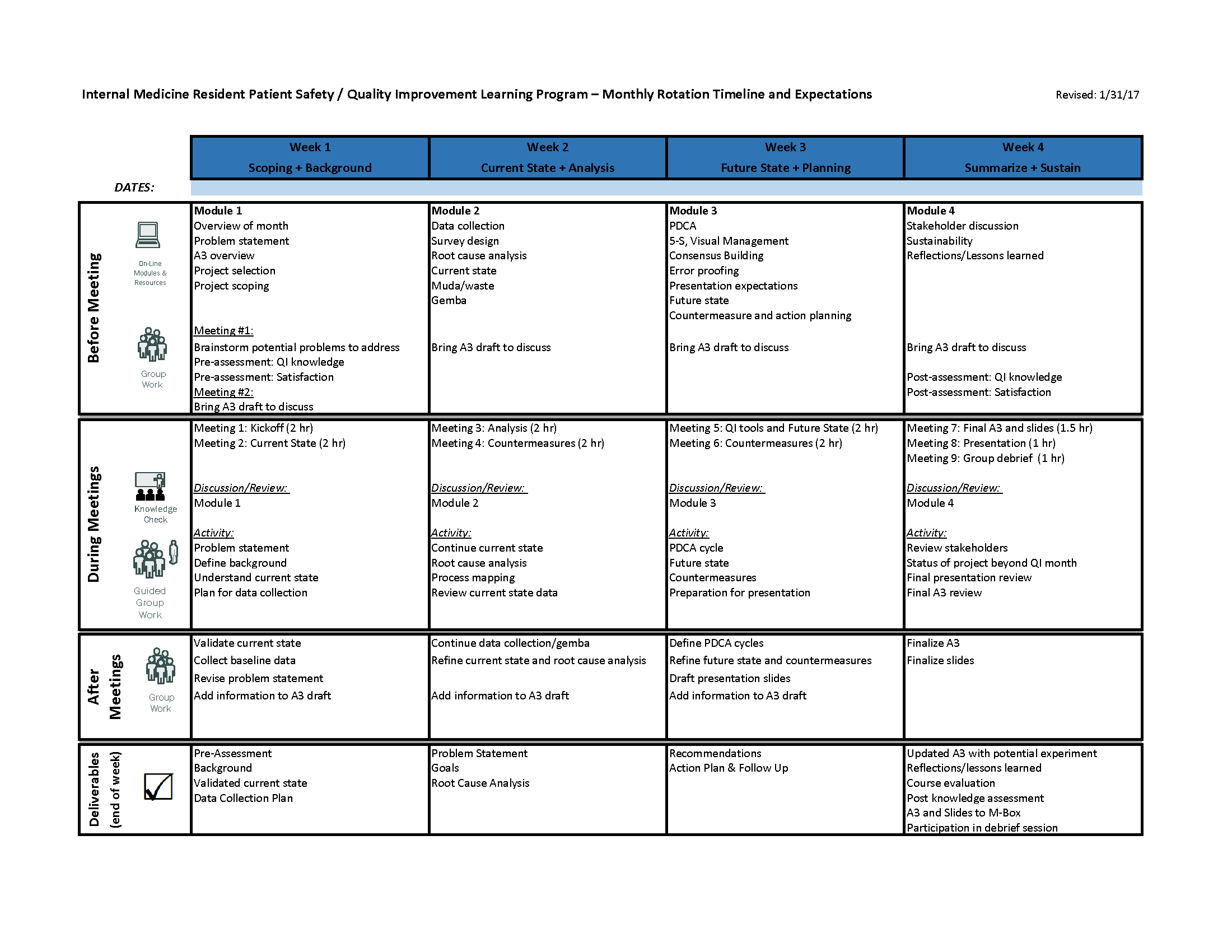
Description: The leaders of the IMRP’s patient safety and quality curriculum conducted a thorough investigation into the current state of the curriculum through interviews with faculty facilitators, GME leadership, members of the house officer quality and safety council, chief medical residents, and residents in the program. A formal needs assessment and gap analysis were conducted. Residents reported that group project work was an effective method by which to learn the principles of safety and quality, but that with limited time, it remained difficult to identify appropriately scoped projects and continue projects through the intervention stage. As a result, the IMRP partnered with the Performance Improvement Team. This group, comprised of experts in engineering, co-facilitated alongside physician leaders to assist resident groups with choosing appropriate projects, provide structured lean methods coaching and A3 guidance (see Figure), rapidly connect teams with institutional resources, and collaborate on resulting scholarship and dissemination both locally and nationally. Resident teams surveyed before and after the project month reported a 34% overall improvement in knowledge of various topics in safety and QI. Two teams in 6-months had posters accepted to national conferences. Quality of A3 documents, as measured by a project evaluation tool, increased substantially after co-facilitation with Performance Improvement Team members began.
Conclusions: Embedding engineering experts in patient safety and QI into residency programs’ teaching efforts creates a multidisciplinary team focused on aligned institutional initiatives. This partnership results in improved resident satisfaction with patient safety and QI training, higher quality group project work with higher likelihood of intervention implementation and dissemination.