Background: Prior studies have shown that miscommunication between providers and families with a non-English language preference (NELP) has been associated with medication errors, inadequate follow-up, increased ED usage, and hospital readmissions. They have also noted barriers to providing translated instructions, such as difficulty with translation, limited resources, and inconsistent use of services. Specifically, our institution did not have a streamlined way to process and distribute translation requests.
Purpose: To create an innovative prioritization system for translating patient education materials within our health system.
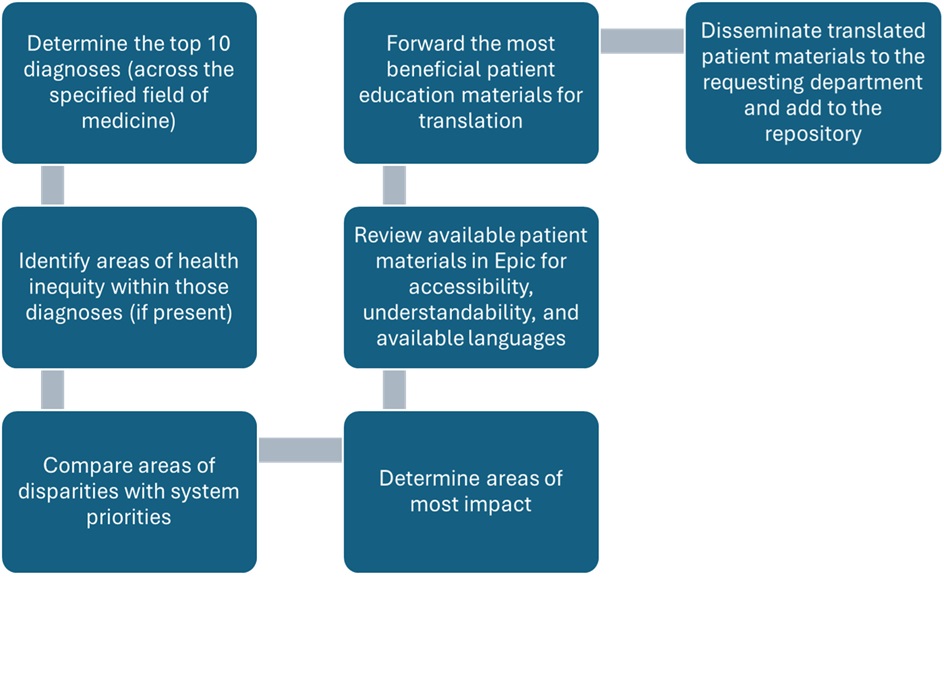
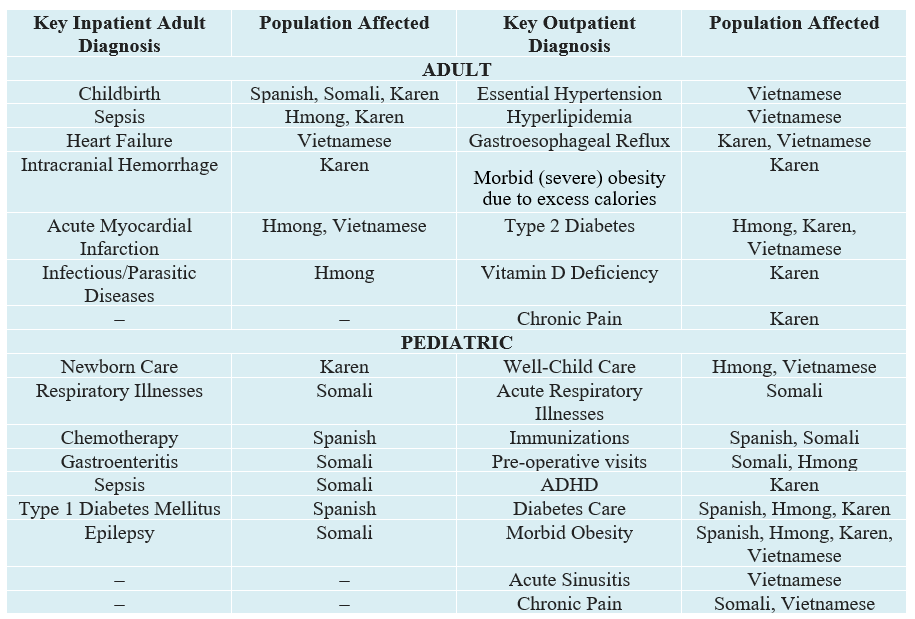
Description: We first determined the most common languages in our health system, followed by identification of medical diagnoses with the greatest prevalence using Epic SlicerDicer. We then evaluated for health outcome disparities between English-speaking and NELP patients using PowerBI, stratifying based on the highest readmission risk, length of stay, and morbidity/mortality. Focus areas for educational intervention were identified based on the most common diagnoses, screening and outcome measures, and system priorities (Figure 1).Our system’s most common languages were Spanish, Somali, Hmong, Karen, and Vietnamese. Within our adult population, the most common diagnoses were pneumonia, heart failure, cirrhosis, and colon cancer & breast cancer screening. In comparison, the most common diagnoses within our pediatric population were newborn care, respiratory illnesses, dehydration from viral illnesses, well-child care (including immunizations), and sick visits for viral respiratory infections. Notably, some diagnoses had higher rates among our NELP population (Table 1). Cross-referencing with system priorities and quality measures, our pilot educational interventions will focus on colon and breast cancer screening, heart failure, childhood vaccines, newborn care, and respiratory illnesses.
Conclusions: Creating a process to optimize translating patient education materials for non-English speaking families reduces disparities and promotes improved care. Future goals will focus on translating written education and creating audiovisual education for these areas in our system’s most common languages, piloting the implementation of these materials, and assessing the effectiveness of our prioritization and implementation process.