Background: Patient education was emphasized in the updated Centers for Disease Control and Prevention’s educational core element for hospital antibiotic stewardship. Despite this, it is not known what education patients receive prior to discharge or if they are being effectively engaged in antibiotic stewardship efforts. Patients’ perceptions and beliefs about antibiotic use and resistance may have an impact on compliance with therapy and desire for additional antibiotics in the future. Understanding the patient experience may lead to more effective ways to involve them in antibiotic stewardship programs at transitions of care. Therefore, we aimed to determine the effectiveness of antibiotic education provided during hospitalization, as well as patient beliefs and knowledge regarding antibiotic use and antibiotic resistance following discharge.
Methods: We performed telephone surveys of a convenience sample of patients discharged from a single academic tertiary facility between August and November 2019. Patients were eligible for inclusion if they had been included in an intervention to improve antibiotic prescribing at discharge. Patients were excluded if they were re-admitted at the time of follow-up, were unable to speak on the telephone, or had a nonworking telephone number. Patients were contacted by phone (3 attempts) 7-14 days after discharge. After obtaining verbal consent, patients were surveyed about their recent experience with antibiotics, the education they received about antibiotics during admission, and their understanding of antibiotic use and antibiotic resistance. Findings were summarized using descriptive statistics.
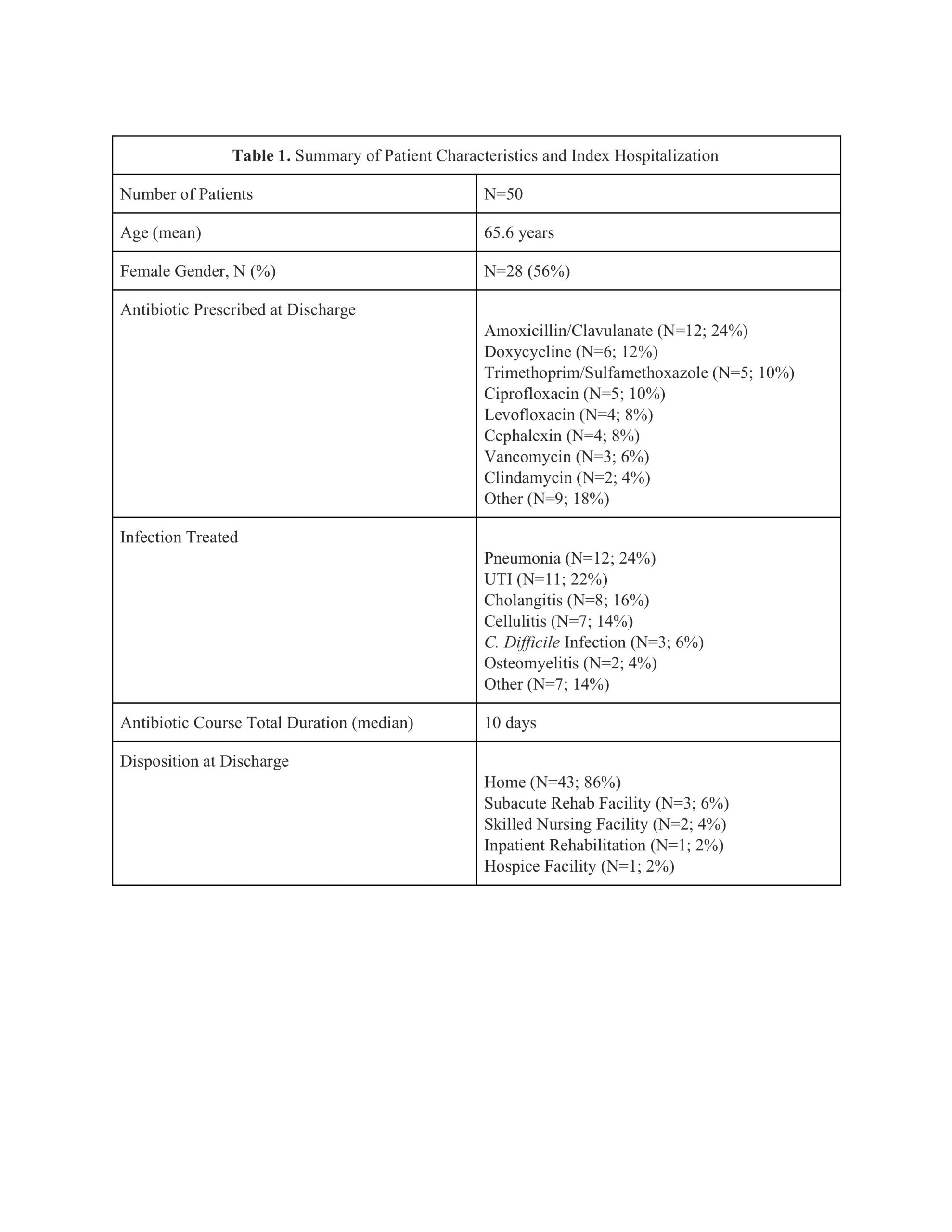
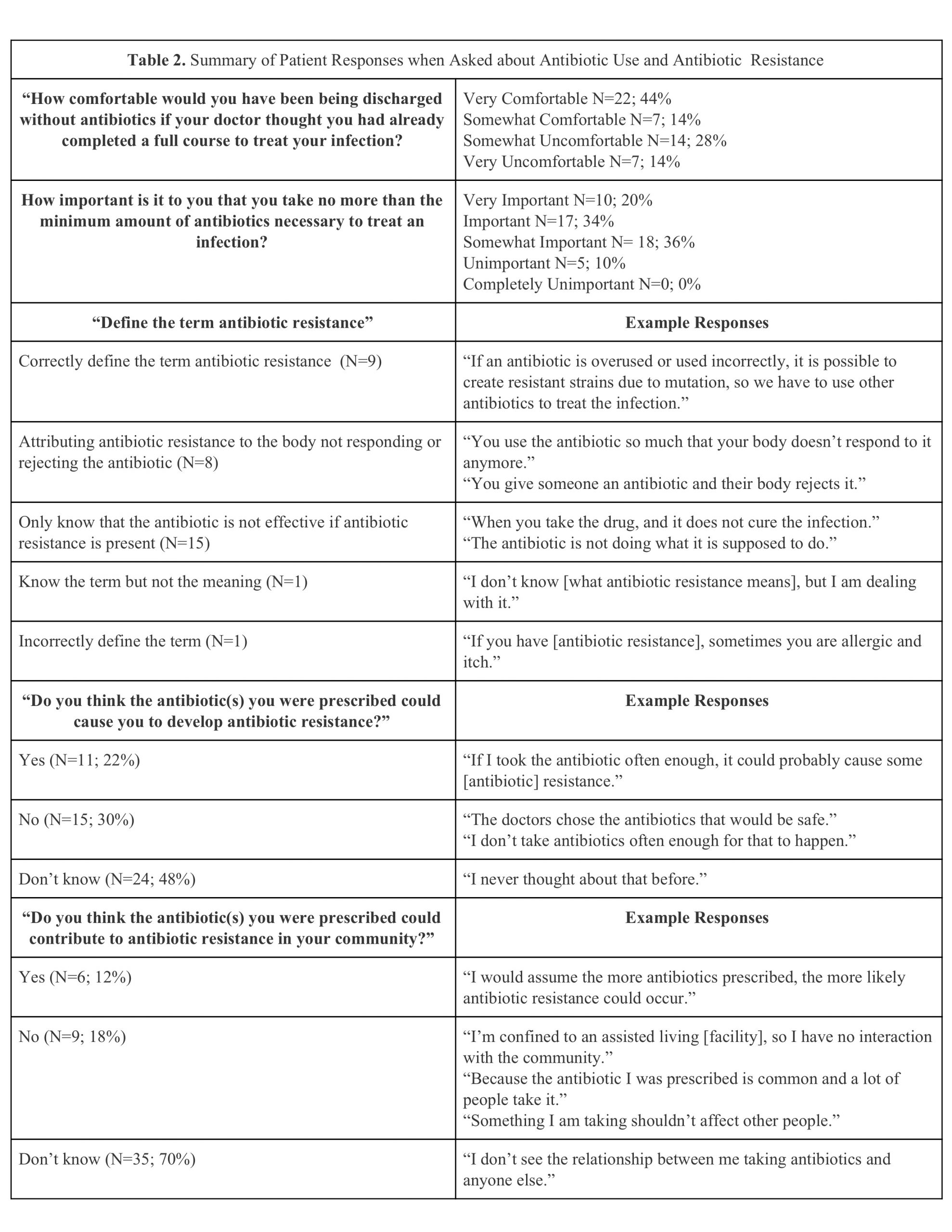
Results: Of 81 patients eligible for inclusion, 50 (62%) were reached by phone and agreed to participate in the survey (Table 1). Though 56% of respondents reported discussing the prescribed antibiotic(s) with a medical professional prior to discharge, few recalled reviewing possible side effects (28%) or potential medication interactions (10%). Only 14% recalled hearing the term “antibiotic resistance.” Most patients (58%) wanted to receive more education when being prescribed a course of antibiotics via discussion with a clinician (90%) and/or supplemental reading material (60%). Patients’ beliefs about antibiotic use and knowledge regarding the development of antibiotic resistance were evaluated (Table 2). When asked about antibiotic resistance, only 26% could correctly verbalize this term’s meaning. When asked about potential sources of antibiotic resistance, 44% were not able to name any possible causes. Approximately one-third (38%) felt that resistance was a significant or very significant problem, and few thought that the antibiotics they were prescribed could increase resistance in themselves (22%) or their community (12%).
Conclusions: About half of patients did not recall discussing antibiotics with a medical professional during hospitalization, and those that did, rarely remembered details. Furthermore, patients’ understanding of antibiotic resistance was poor as few patients felt taking antibiotics could lead to resistance, and most could not correctly define the term or name possible causes of antibiotic resistance. Encouragingly, most patients wanted to become engaged in their care and learn more about the antibiotics they were being prescribed. This insight creates an opportunity to involve patients in hospital antibiotic stewardship efforts while hospitalized and at discharge.