Background: Opioids are widely prescribed for cancer and non-cancer related pain in hospitalized patients. The opioid usage increased roughly three times in the past two decades. Pain is a feeling of distress evoked by sensory stimuli with/without organ damage and an associated emotional experience. Considering the subjective nature of pain, the need for medication is often unclear and the physician’s ability to provide adequate pain control is often limited. In National Survey on Drug Use and Health (NSDUH), 50.5% of people misused prescription painkillers from a friend or relative and 22.1% from their physician.
Methods: A retrospective cohort study was conducted by including all patients (n=1739) from our Internal Medicine admissions database for a one year time period between 2016 and 2017. The patient data on demographics, non-medical opioid usage, opioids prescribed in hospital, medical indications for which opioids were prescribed and discharge opioid prescription information were collected.Design
Prescribed opioid exposure:
We defined prescribed opioid exposure as use of at least one opioid medication during the hospital stay.
Covariates of Interest:
The association between patient characteristics and opioid use during the hospitalization was analyzed. Patient characteristics of interest included: 1. Demographic variables – age, gender, ethnicity 2. Intake of prescribed opioids 3. Illegal drug abuse.
Statistical Analysis:
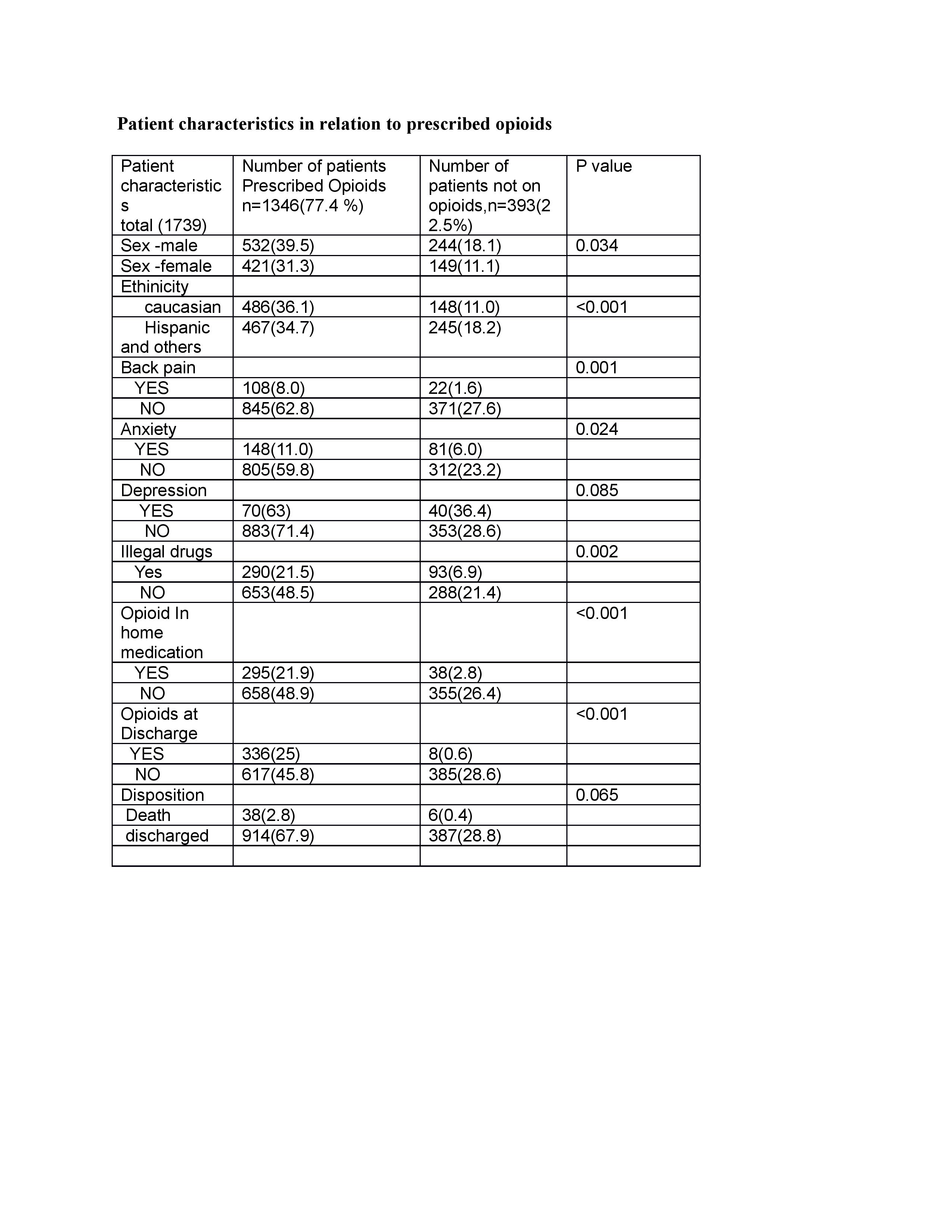
Pearson Chi-square test was used to assess the differences in patient demographics when opioids were prescribed using SPSS version 22 (IBM Corp., Armonk, NY).
Results: 77.4% of all admitted internal medicine patients were prescribed some form (Intravenous, Oral) of opioid medication irrespective of primary and secondary diagnoses. When patients with comorbidities of back pain, anxiety and depression were hospitalized, they received opioid medication at the rate of 83.07%, 64.06% and 63.63% respectively. Caucasian females (35.38% of all patients with back pain) were twice likely to receive opioids during hospitalization than any other race or gender. Patients with prior use of prescribed opioids (24.7% of all inpatients) were seven times more likely to receive opioids in hospital. There was no conscious attempt to reduce opioid prescriptions for patients consuming some form of illegal substance (28.4% of all inpatients) and they were three times more likely to receive opioids during hospitalization. The death rate was high by a factor of seven with opioid usage during hospitalization.
Conclusions: The opioid exposure for hospitalized patients was very high and serious attempts to reduce the exposure is a priority and immediate active intervention is required for changing the physician prescribing practices. Using Opioid Risk Tool and multimodal approach to pain management could reduce the opioid exposure during hospitalization.