Background: The three most common childhood-onset chronic conditions for which adolescents and young adults (YA) use pediatric hospitals are congenital heart disease (CHD), cystic fibrosis (CF), and sickle cell disease (SCD). Existing studies do not establish clear clinical benefits to continued pediatric hospitalization over hospitalization at adult hospitals. We aimed to determine if if continued pediatric hospital use by YA 22-35 years differs significantly 1) across different specific conditions CF, CHD, or SCD; and 2) within each condition by sociodemographic factors (e.g., race, payer)
Methods: We conducted a retrospective cross-sectional analysis of all acute care hospitalizations for YA ages 22-35 years with CF, CHD, and SCD in the 2016-2020 Agency for Healthcare Research and Quality’s (AHRQ) National Inpatient Sample (NIS). Individuals with CHD, CF, and SCD were identified by ICD-10-CM diagnosis codes. We applied survey weights using AHRQ NIS methods to produce nationally representative estimates. Pediatric hospitals were identified using a validated and published classification scheme. To determine if a specific childhood-onset condition or sociodemographic factors were associated with delayed inpatient transition for these YA (as defined by hospitalization at a pediatric hospital >21 years), we used multivariable logistic regression with separate models for the different objectives.
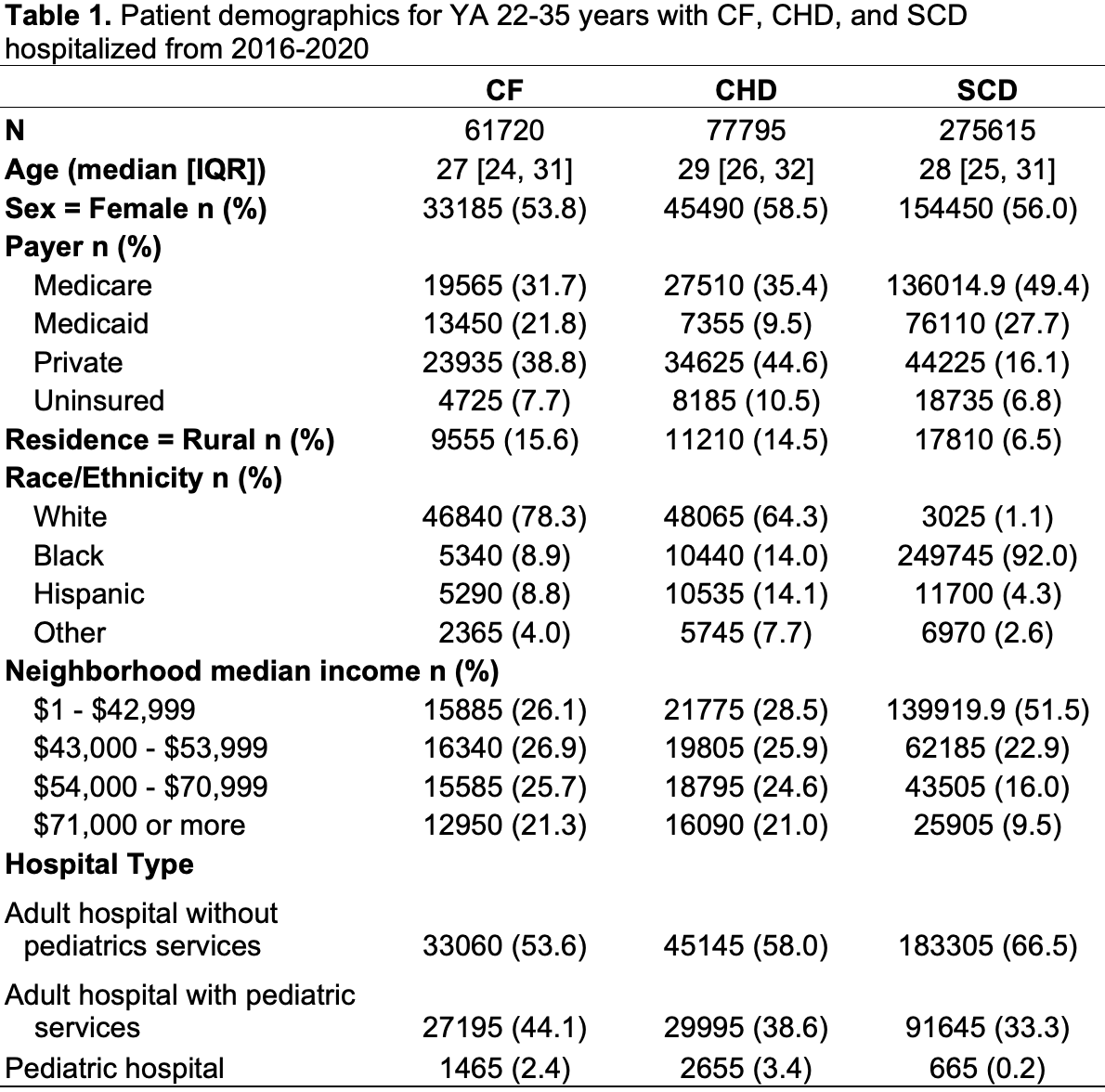
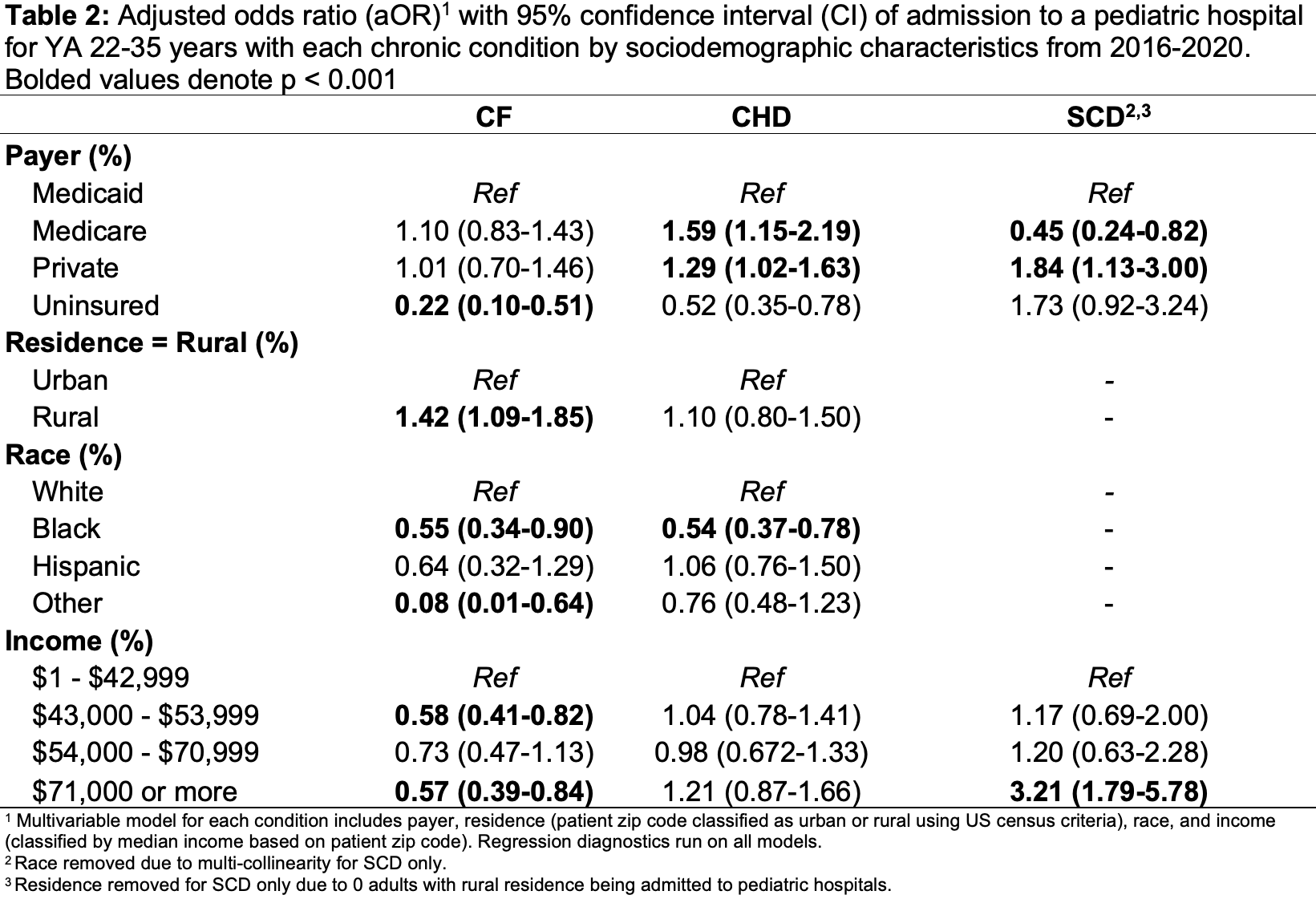
Results: We identified 415,130 total admissions of YA ages 22-35 years with CHD, CF, and SCD of which 4,785 were to pediatric hospitals (Table 1). Comparing across conditions, YA ages 22-35 with SCD were associated with significantly lower odds of admission to a pediatric hospital (aOR 0.17; 95% CI [0.09-0.31]) compared to those with CF (reference group) in adjusted analyses. In contrast YA with CHD had significantly higher odds (aOR 1.50; 95% CI [0.96-2.32]) of pediatric hospital use compared with YA with CF. Relationships between sociodemographic variables and pediatric hospital use varied by condition (Table 2). Black YA with both CF and CHD had significantly lower odds of pediatric hospitalization than white YA. For SCD only, despite 17,810 (6.5%) of YA hospitalizations having rural residence living, zero (0) hospitalizations were in pediatric hospitals.
Conclusions: YA with SCD utilize pediatric hospitals less commonly than YA with either CF or CHD. YA race and residence were associated with pediatric hospitalization use, which may reflect systemic bias within pediatric to adult healthcare transition programs.