Background: Pediatric hospitalists are responsible for educating varying levels of learners while overseeing rounds to deliver high-quality care in an inpatient setting. While many teaching techniques are described, impactful teaching during rounds is a skill not always taught in training. Efficient utilization of teaching techniques is an endeavor that requires tutelage, repetition, and strategic practice. Peer observation offers a mutually beneficial collaboration in which the effective use of teaching techniques during rounds can be observed, evaluated, and discussed to reinforce helpful strategies. Objective: Evaluate the change in comfort level and perceived frequency of teaching methods utilized by pediatric hospitalists after completing a peer observation program of clinical rounds.
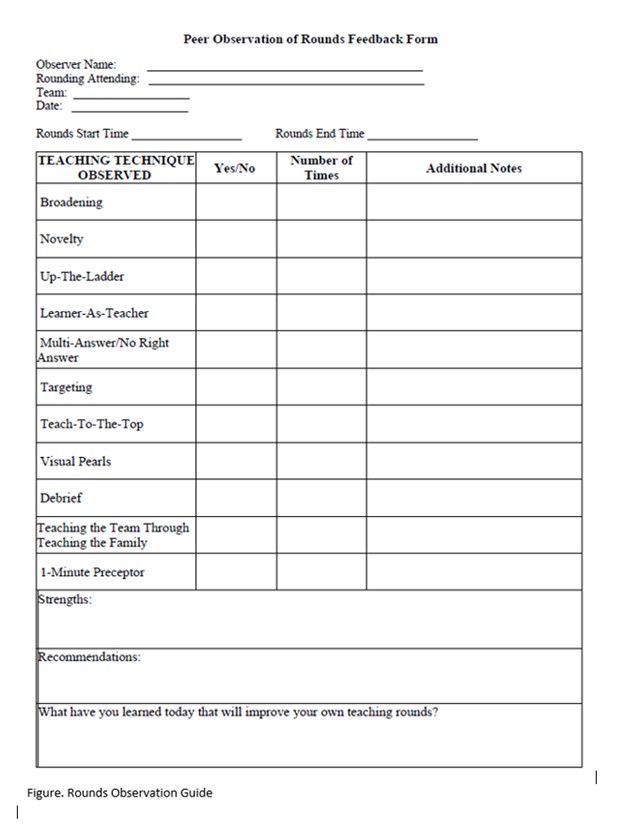
Methods: This prospective observational study was conducted at a tertiary care pediatric hospital between 7/2022-7/2023. The program was voluntary and incentivized. All pediatric hospital medicine division members were eligible to participate. Participants attended a preliminary didactic session to define eleven formal teaching methods and completed a pre-survey evaluating participants’ comfort level and perceived utilization frequency of these teaching techniques. Program participants then observed three individual bedside rounding sessions involving hospitalists at varying levels of experience: Tier (T) 1, < 6 years post-training; T2, 6-11 years; and T3, >11 years. Witnessed teaching methods were recorded by observers using a rounds feedback form (Figure). A post-rounds debrief involving the observer and rounding hospitalist followed each session. After three individual sessions, a post- program survey was completed by participating hospitalists assessing comfort level and perceived frequency of teaching techniques used. Pre- and post-program surveys were collected and analyzed utilizing descriptive statistics, Chi Square, and Kruskal Wallis test.
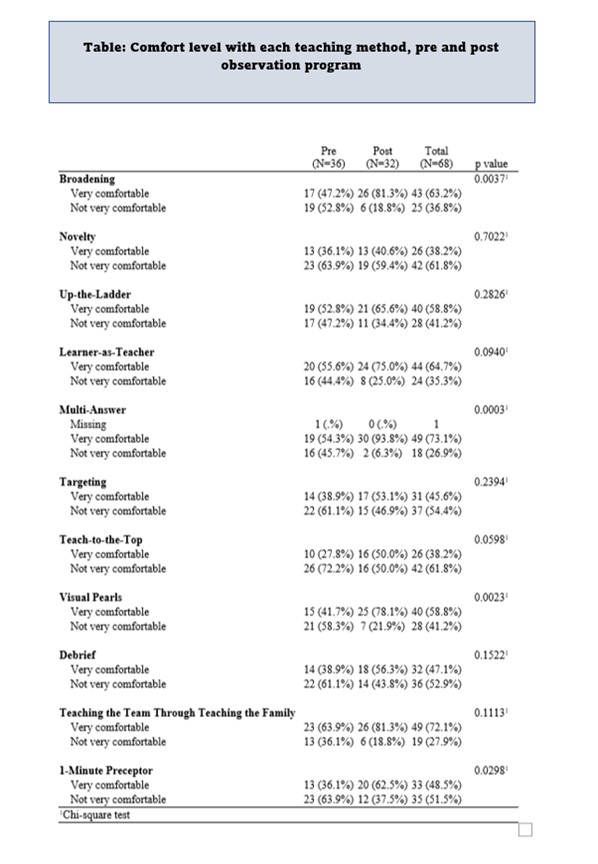
Results: 31 of 48 eligible participants completed the program. 93 observations occurred with 32 in T1, 28 in T2, and 33 in T3. Participant comfort level improved in 10 of the 11 learned teaching techniques after program completion, with four reaching statistical significance (Broadening (p=0.0037), Multi-Answer (p=0.0003), Visual Pearls (p=0.0023), 1-Minute Preceptor (p=0.0298) (Table). When assessed by tiers of experience, comfort level in teaching improved in 8 of 11 (T1), 9 of 11 (T2), and 7 of 11 (T3) participants. Statistical significance was demonstrated for Multi-answer in T1 and T3 (p=0.004 and p=0.04), respectively. The perceived frequency of utilization pre- and post- program completion was not statistically different for any teaching technique overall or when analyzed by tier, with the exception of the Multi-Answer technique in T1 (p=0.0147) (Table).
Conclusions: Increased participant comfort level using a majority of teaching methods was noted after completing a peer observation program evaluating teaching on rounds. However, the perceived frequency of technique utilization remained essentially the same prior to and after program completion. The findings suggest that evaluative observation of rounds is a beneficial tool in promoting increased attending comfort with varied teaching strategies and may be helpful in creating a more effective learning environment. Future studies will evaluate the perception of teaching strategies from the learner perspective.