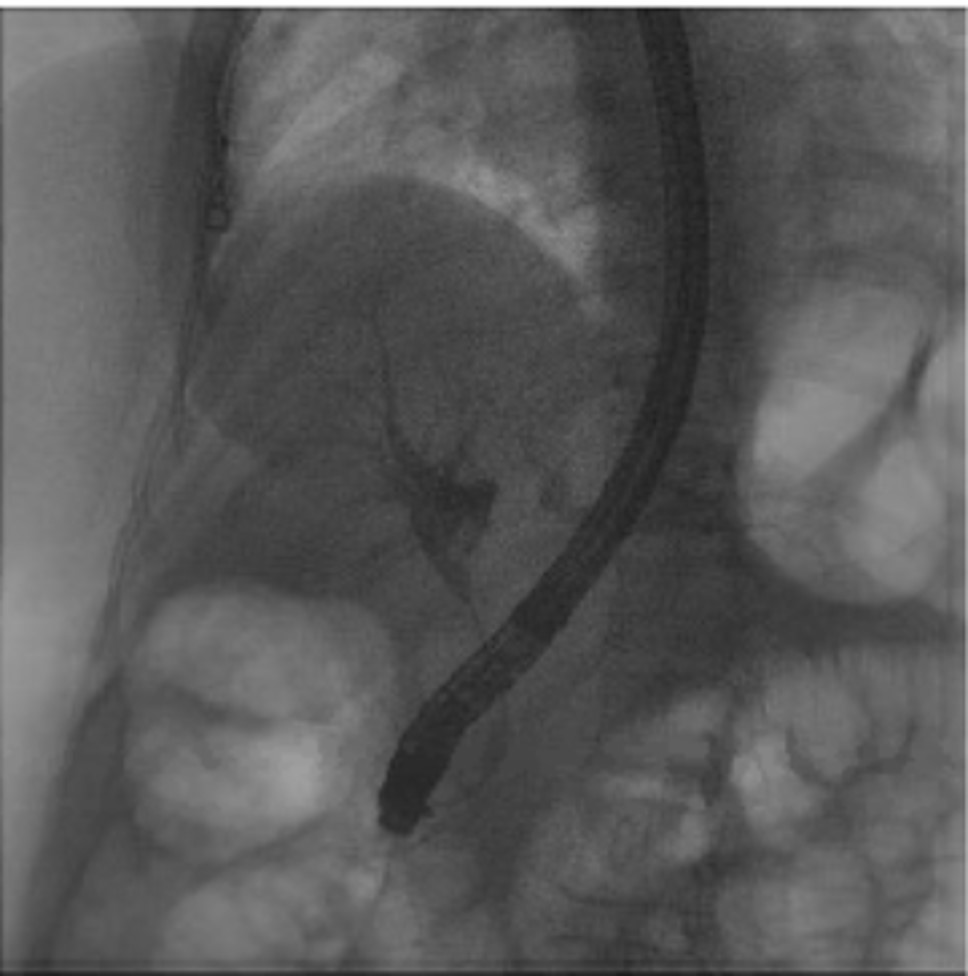
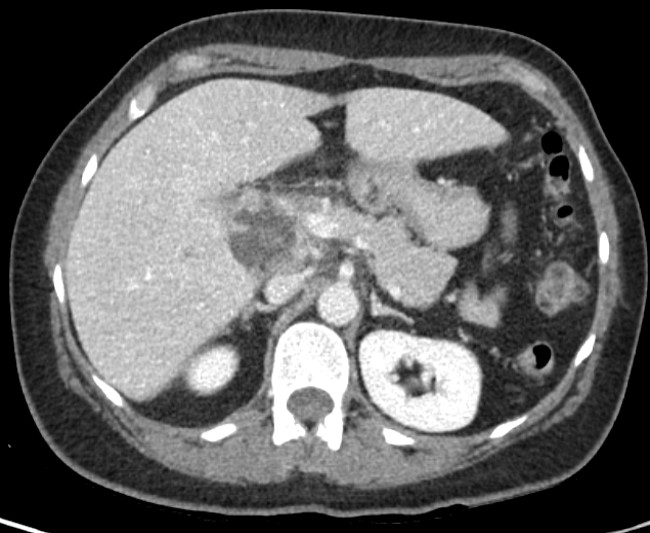
Case Presentation: We present a 42-year-old Caucasian female patient who presented with tea-colored urine noted during a new employment urine drug test associated with waxing and waning sharp epigastric pain for few months prior to presentation. Her medical history was negative for abdominal trauma or any prior surgeries. On physical exam, there was no fever and her vital signs were within the normal range. Patient had mildly icteric sclerae, negative murphy’s sign, soft nontender abdomen. Labs were notable for bilirubin 3.7, alkaline phosphate 566, ALT 315, AST 127, WBC 10.4, lactic acid 1.3.Abdominal ultrasound imaging revealed cholelithiasis and biliary duct dilation. Contrast enhanced CT of her abdomen and pelvis was significant for a pancreatic head mass with obstruction and dilation of the intrahepatic and extrahepatic ducts. Endoscopic retrograde cholangiopancreatography (ERCP) showed a biliary stricture (~2.5cm in length) secondary to external compression from multi-loculated biloma, a collection of bile fluid outside of the gallbladder, suggestive of prior perforation. Pancreatic head mass was ruled out. General surgery was consulted for cholecystectomy. During surgery, the patient was found to have purulent cholecystitis with an abscess adjacent to the infundibulum of the gallbladder and phlegmon surrounding the cystic duct with dense adhesions. A subtotal cholecystectomy was performed with staples due to extensive inflammation. A Jackson-Pratt drain was removed 2 days post-op. There was notable improvement in bilirubin and transaminases. Biliary gastroenterologists recommended a repeat ERCP in 2 months for biliary stent removal.
Discussion: Cholecystitis is inflammation of the gallbladder, secondary to obstruction of the cystic duct by gallstones in 90% of cases. Risk factors include female sex, obesity, increased age, and pregnancy. It is more common among people of Scandinavian descent, Pima Indians, and Hispanic populations. In the United States, Caucasians have a higher prevalence of cholecystitis than African Americans. Initial treatment includes hydration, intravenous antibiotics (piperacillin-tazobactam, ampicillin-sulbactam, or meropenem), and analgesia. There is evidence that the best outcomes occur when a laparoscopic cholecystectomy is performed within two days of presentation (Zafar et al). 10-15% of patients will have perforations, increasing their mortality rate to 50-60%. Often, perforations will cause a collection of bile fluid in the abdominal cavity, which can cause infection and further complications. Our patient likely had a gallbladder perforation at an unspecified time in the past year. It is important to consider biloma on the differential for a young patient presenting with a pancreatic head mass.
Conclusions: Acute cholecystitis can present in different ways for patients. Some may present early with right upper quadrant pain, while others may present with tea-colored urine after a perforation.Review all imaging to ensure accurate diagnosis prior to verbalizing potential diagnoses to patients.Further research is necessary to determine the comparison in the imaging of multiloculated bilomas and pancreatic head masses.