Background: Current guidelines recommend continuing aspirin during elective non-cardiac surgery in 1) patients with prior percutaneous coronary intervention (PCI) if the bleeding risk allows and 2) patients without prior PCI if thrombotic risk outweighs bleeding risk. Comparing the risk of thrombosis and bleeding is frequently inexplicit, particularly in low and intermediate bleeding risk surgery. The practice pattern of preoperative antiplatelet interruption in low and intermediate bleeding risk surgery/procedure and postoperative adverse events is limited in real-life practices.
Methods: We extensively reviewed data of patients taking both single and dual antiplatelet therapy (DAPT) hospitalized for elective low and intermediate bleeding risk noncardiac surgery/procedure during January 2020 to October 2021 in a teaching hospital. The exclusion criteria were concomitant anticoagulant therapy and any bleeding disorder. All demographic data, indication of antiplatelet therapy, perioperative antiplatelet management, duration of antiplatelet interruption. The outcomes between 2 groups of patients were collected and analyzed: stopping all antiplatelet medications before surgery/procedure (STOP) and continuing at least one antiplatelet medication before surgery/procedure (CON).
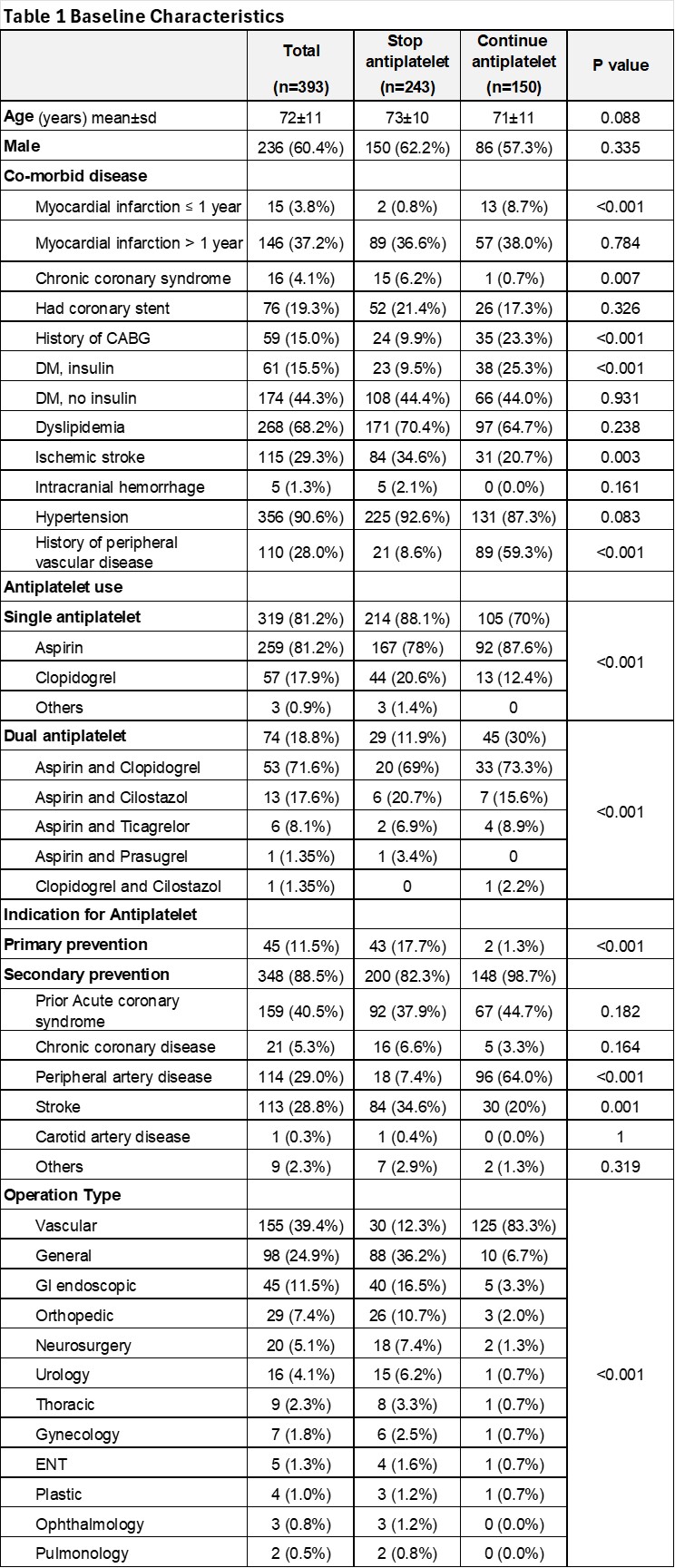
Results: Of 5,091 hospital admissions of patients taking antiplatelet therapy hospitalized for noncardiac surgery/procedure, 393 patients met our criteria. Two hundred and thirty-six (60.4%) were men and the mean age was 72 years. Three hundred and nineteen patients (81.2%) took a single antiplatelet (SAPT) and 17 (18.8%) took DAPT. Three hundred and twenty (81.4%) patients underwent low bleeding risk surgery. Three hundred and forty-eight (88.5%) of the participants took antiplatelet for secondary prevention. The patients were classified into STOP group 243 patients (61.8%) and CON groups 150 patients (38.2%) as shown in Table 1. The median duration of antiplatelet interruption before surgery/procedure was 7 (6,8) days and 0 (0,0) days in the STOP and the CON groups. The median duration of antiplatelet restart after surgery/procedure was 4 (2,7) days and 0 (0,0) days in the STOP and the CON groups. The total duration of antiplatelet interruption was 12 (8.25,15) days and 0 (0,0) days in STOP and CON groups, respectively. The numbers of major adverse cardiac events (MACE), including acute myocardial infarction (AMI), stroke, or cardiovascular death, in the STOP and the CON groups after surgery/procedure: within 15 days were 7 and 1 (2.9% vs 0.7%, P = 0.162); within 30 days were 10 and 1 (4.1% vs 0.7%, P = 0.044), and within 90 days were 12 and 1 (4.9% vs 0.7%, P = 0.021), respectively. The major bleeding events in the STOP and the CON groups after surgery/procedure: within 15 days were 7 and 5 (2.9% vs 3.3%, P=0.80), within 30 days were 9 and 5 (3.7% vs 3.3%, P = 0.044), and within 90 days were 10 and 6 (4.1% vs 4.0%, P = 0.955), respectively as shown in Table 2.
Conclusions: In real-life practices, interruption of all antiplatelets preoperatively in low and intermediate bleeding risk, elective noncardiac surgery is common and is associated with higher postoperative MACE with comparable postoperative major bleeding.