Background: Post hospital discharge review during the transition from hospital to skilled nursing facility (SNF) is critical to avoid medication errors, improve patient outcomes and reduce hospital readmissions (1-3). Despite increased integration of electronic health records (EHR) across health entities, communication gaps and discharge-related medication errors still persist (2,4). These challenges can be more predominant with SNFs given silos of care between physician practices and EHRs. A multidisciplinary team approach including a pharmacist has been shown to reduce readmissions and promote safety through medication reconciliation, optimization, and monitoring (5). The Duke Population Health and Management Office “TeleHOPE” (Hope Optimization Program for Elders) program was created to bridge this gap. This program promotes collaboration across care transitions via a weekly telehealth videoconference (6). With access to both the discharge hospital’s electronic health record and the SNF medication administration record (MAR), the pharmacist has a unique opportunity to provide real time recommendations and resolve medication discrepancies.
Methods: Patients discharged from 2 academic hospitals to all 3 participating skilled nursing facilities are reviewed weekly by our health system multidisciplinary team composed of a pharmacist, geriatric nurse practitioner, hospitalist and learners from various health disciplines. The SNF team is composed of a director of nursing, social worker, and advanced practice provider. Hospitalization records are reviewed by the TeleHOPE team for transitional care needs, geriatric syndromes, treatment plans, and goals of care. The pharmacist review focuses on medication history, appropriateness based on indication, monitoring parameters, medication refill history, proper administration at SNF, and length of therapy. The patient status and team recommendations and discrepancies are then discussed with the SNF team and a secure note in the EHR is sent to the patient’s health care team.
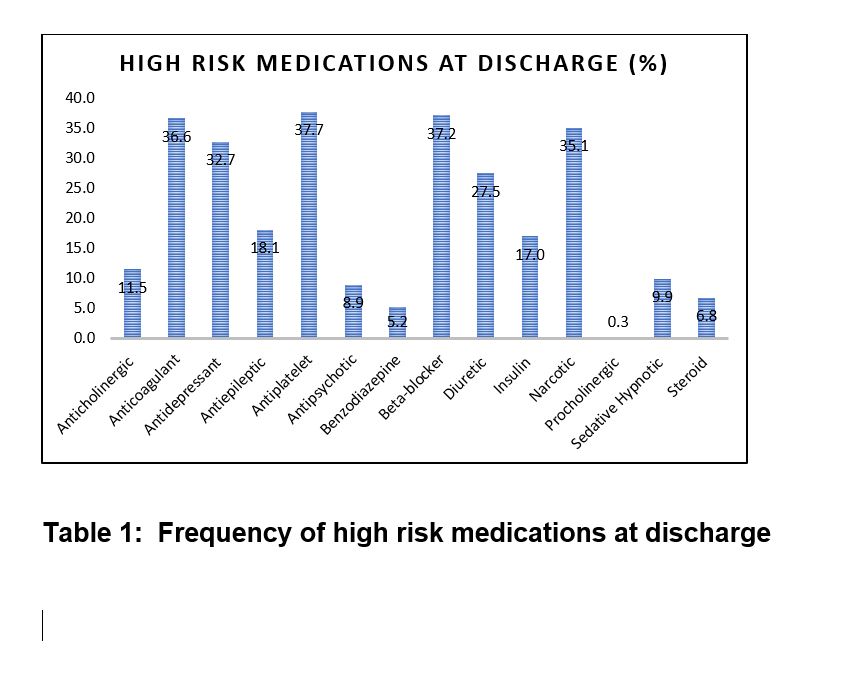
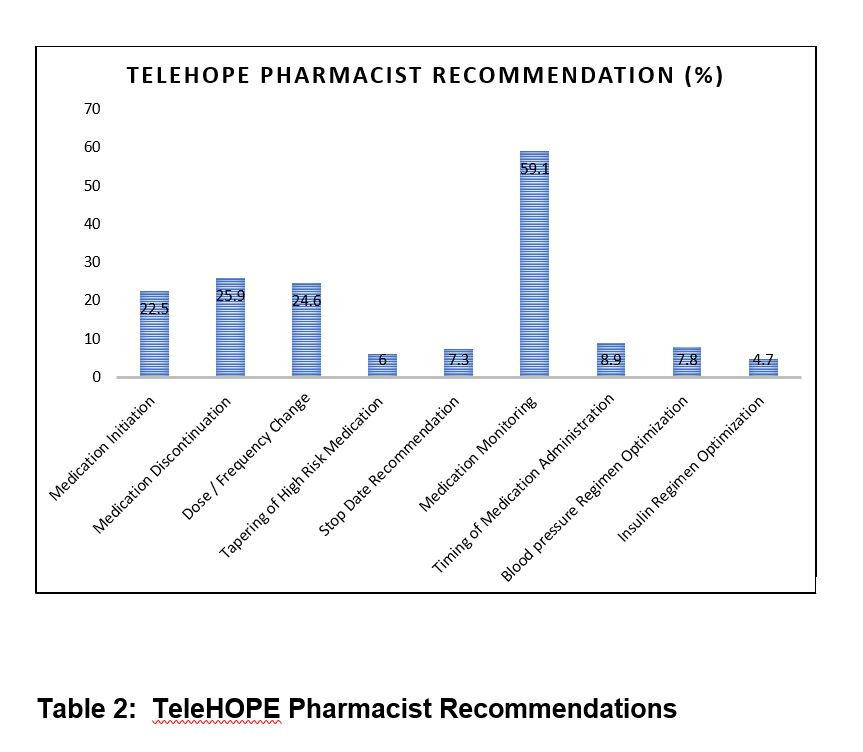
Results: A total of 479 discharges from our hospitals to participating facilities were reviewed by the TeleHOPE program from August 2020 through December 2021. The frequency of high risk medications at discharge are described in Table 1. The most common medication discrepancies identified by the TeleHOPE pharmacist included: unintentional omission (18.8%), improper dose frequency (5.6%), and therapeutic duplication (3.6%). Recommendations by the TeleHOPE pharmacist are described in Table 2. Patients discharged to TeleHOPE facilities had lower readmission rates over this time period as compared to those discharged to non-participating facilities; 7 day (4.8% vs 6.3%); 14 day (7.3% vs 10.8%); and 30 day (16.1% vs 19.3%).
Conclusions: Pharmacist involvement during hospital to skilled nursing transition of care improves identification of high risk medications and discharge related medication discrepancies. With access to the electronic health record from both the discharging hospital and the SNF, the pharmacist has a unique perspective and is able to provide therapeutic recommendations for medication optimization. In addition, the implementation of the TeleHOPE program may reduce unplanned readmission rates.