Background: Complex non-pharmacologic interventions containing multiple, or bundled, components can successfully prevent and treat hospital-acquired delirium in older adults. However consistent implementation, and the measurement of compliance, of these bundled interventions can be challenging to sustain in hospital settings especially in presence of COVID-19. Developing workflows with a smaller sub-set of components that are feasible to deliver and where compliance can be easily tracked may hold promise. Therefore, the aims of this study are to: 1) determine the effectiveness of a 5-item daytime and 4-item nighttime nurse-driven delirium reduction workflow on delirium rates and length of stay in hospitalized adults and 2) determine the impact of COVID-19 on this workflow and outcomes.
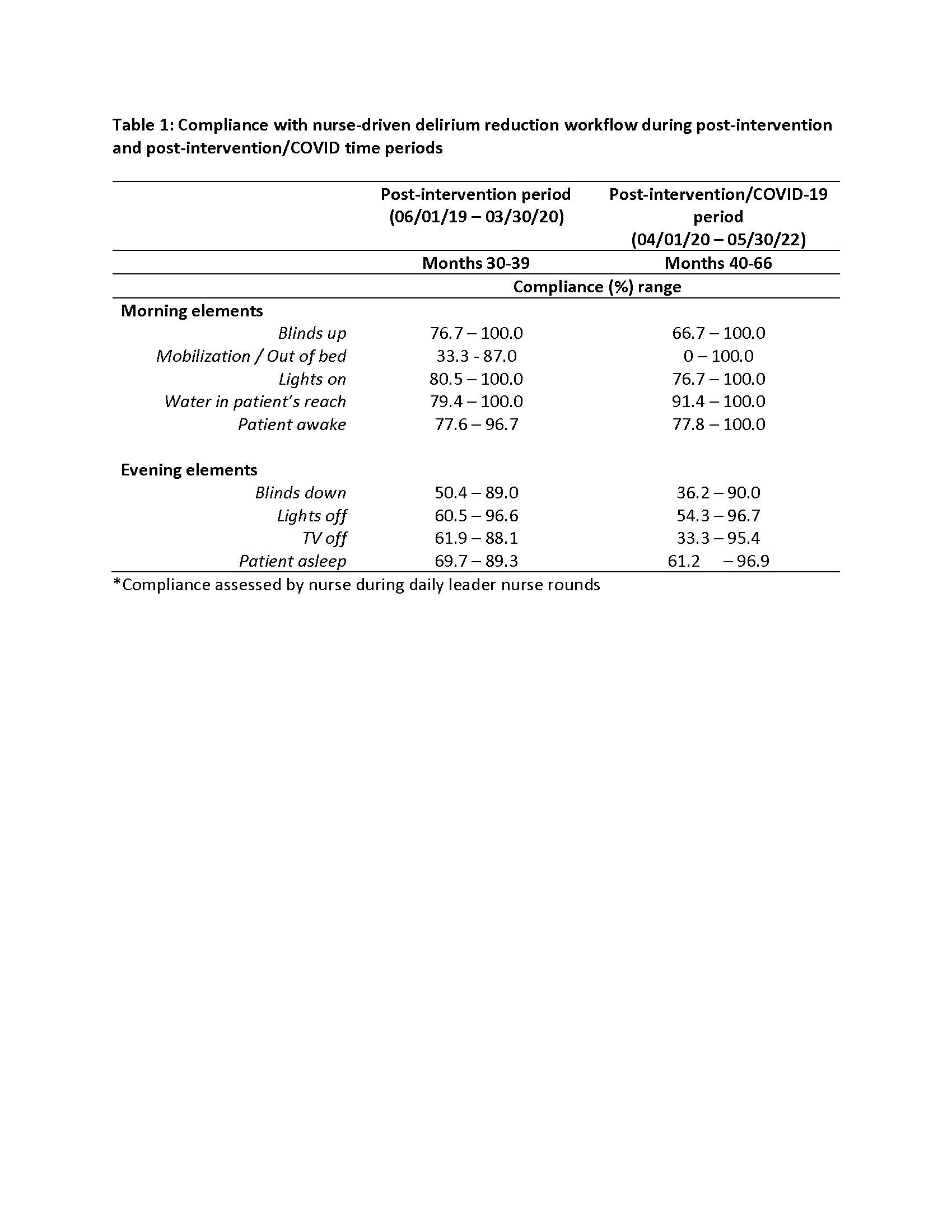
Methods: All patients admitted to the Acute Care for Elders (ACE) Unit at an academic medical center were eligible. We developed a nurse-driven evidence-based workflow that includes: 1) five daytime interventions (promotion of daytime wakefulness – patient room lights on, blinds up, mobilization/out-of-bed, water within patient’s reach, patient awake); and 2) four nighttime interventions (nighttime sleep promotion – patient room lights /TVs off and blinds down, patient asleep). Workflow components were chosen due to feasibility of consistent delivery and were easy to track (i.e., compliance can be observed from outside the room). To evaluate the workflow and impact of COVID-19, we measured compliance with workflow components during daily leader rounds using an online data capture survey tool (a ≥80% compliance benchmark for each item was set). Workflow compliance data was feedback monthly to unit staff. We then conducted an interrupted time series analyses to determine change in the trends of the unit’s delirium rate (i.e., delirium days) and average length of stay (aLOS) for patients with delirium.
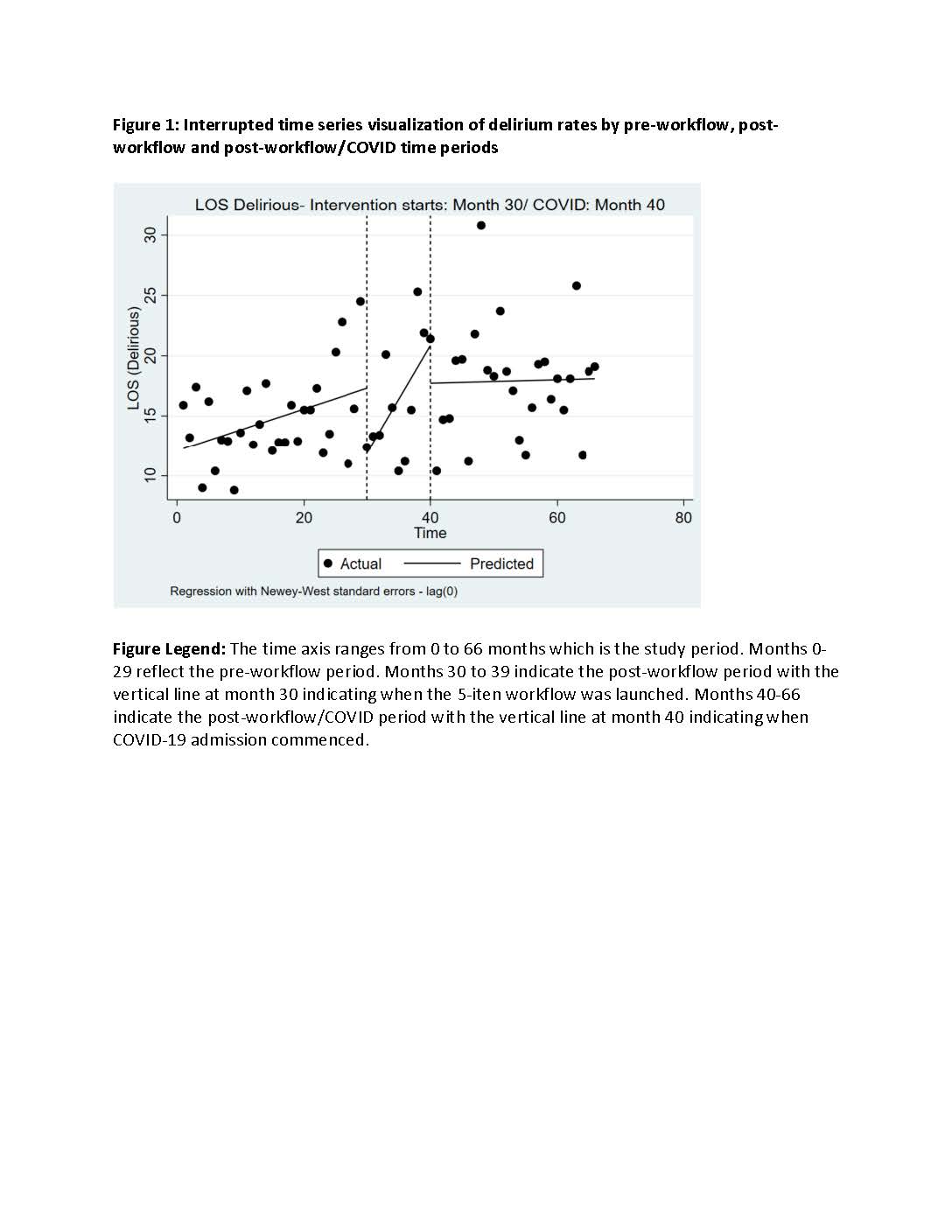
Results: There were 4925 patients admitted to the ACE Unit in the pre-workflow period (Months 0-29; 06/01/17 to 05/31/19), 1640 patients in the post-workflow period (Months 30-39; 06/01/19 to 03/30/20) and 4071 patients in the post-workflow/COVID period (Months 40-66; 04/01/20 to 05/30/22). Compliance with daytime workflow elements remained generally high across both post-workflow time periods (see Table 1). However, adoption of nighttime workflow elements decreased during the post-intervention/COVID period. Following the launch of the workflow, delirium rates significantly decreased at a rate of 12.2 days per month (95% CI = [-11.4, -0.44] and this trend was significantly different than the pre-intervention trend (p< 0.01). This significant decrease in delirium rates was not sustained once COVID-19 patients were admitted to the unit (see Figure 1). After launch of the workflow, there was no significant changes in aLOS for patients with delirium at any time.
Conclusions: Integration of a 5-item daytime and nighttime nurse-driven delirium reduction workflow is feasible to deliver, monitor and positively impacts delirium reduction but not length of stay. The positive effects of on delirium rates were not sustained following the emergence of COVID-19 potentially due to the high risk of delirium associated with COVID-19 and a decrease in compliance with evening workflow components. Future efforts should evaluate strategies to improve workflow compliance that considers the impact of COVID-19 as well as the impact of isolation on delirium rates.