Background: Patients with alcohol use disorder are at high risk of alcohol withdrawal syndrome (AWS) while hospitalized. AWS includes a wide spectrum of clinical features and is associated with significant morbidity and mortality. Pharmacologic treatment of AWS revolves around the use of benzodiazepines (BZDs) or phenobarbital (PHB). Current literature recommends symptom-triggered BZD dosing as first line treatment. Guidelines recommended PHB use when BZDs are contraindicated or for experienced clinicians in settings with closer monitoring due to a theoretical risk of increased sedation. However, PHB has not been associated with clinically significant sedation. Currently, there is limited and conflicting evidence that supports the use of PHB on general medical floors. This study is intended to verify the safety of PHB. We primarily aimed to compare length of stay between patients initiated on PHB compared to BZDs. Secondarily, we studied the need for ICU transfer, 30-day Emergency Department (ED) visits after discharge, 30-day readmission rates, and all-cause mortality.
Methods: This was a retrospective chart review designed to analyze hospital course outcomes of adult patients with alcohol withdrawal or alcohol intoxication. Our team manually reviewed electronic health records of adult patients with a primary diagnosis of AWS or alcohol intoxication admitted to one of two community teaching hospitals between 9/30/2021 and 9/30/2022. Demographic and pertinent clinical data was gathered. Exclusion criteria included patients admitted directly to the ICU, patients transferred from an outlying facility, patients that were pregnant, or prisoners. Patients intoxicated with multiple substances, patients that received an addiction medicine consult, and patients that had an allergy to PHB or another antiepileptic were also excluded.
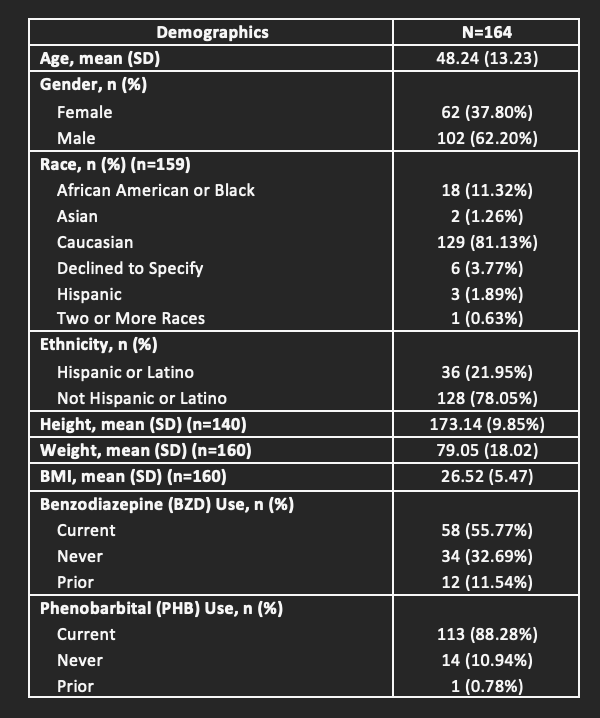
Results: A total of 164 patients were included for analysis. Mean age was 48.24 ±13.23 years and 37.8% were female. Of the 164 patients, 106 were treated with PHB, 51 with BZDs, and 7 transitioned from BZDs to PHB. There was no significant difference in length of stay (LOS) between patients treated with PHB compared with BZDs (p-value = 0.080). There was a significant difference in the number of patients that needed ICU transfer who transitioned from BZD to PHB (p-value = 0.005). There was no significant difference in the remaining secondary outcomes of all-cause mortality, 30-day readmission rates, and 30-day ED visits.
Conclusions: Our study did not find a significant difference in LOS, 30-day ED visits, 30-day readmissions rates, or all-cause mortality between the two treatment groups. However, we observed a notable increase in ICU transfers when patients were transitioned from BZDs to PHB. This potentially was the result of an underestimation of withdrawal severity on admission. Moreover, there was no significant difference in ICU transfers between PHB and BZD groups overall, which helps to support the safety profile of PHB utilization. These results are supportive of existing data that PHB should be considered a safe alternative to BZD when treating severe AWS. Study limitations include a low number of ICU transfers, and further studies should be conducted evaluating the safety and efficacy of transitioning from BZD to PHB.