Background: Since the 1960s, benzodiazepine therapy has been the standard of care for alcohol withdrawal syndrome (AWS) [1]. Recently, phenobarbital-based withdrawal has re-emerged as a potentially safer and more effective option that can decrease admission rates when given in the emergency department (ED) [2-7]. Thus, many academic medical centers (AMCs) have switched to phenobarbital for AWS. Barriers to implementation include provider familiarity and concern for respiratory depression [8]. Moreover, to be effective, phenobarbital is often administered at high weight-based doses (10mg/kg) which can make providers uncomfortable [2-7]. These barriers may be more pronounced in rural hospitals where there is often no intensivist support or association with AMCs that promote practice changing initiatives. There are no studies describing its use or implementation in a rural setting. Here, we describe an initiative to bring phenobarbital treatment of AWS to an ED at a rural medical center through implementation of a practice changing protocol.
Purpose: Our goal was to increase the use of phenobarbital for the treatment of AWS in a rural ED with the specific aim to increase comfort with high weight-based dosing.
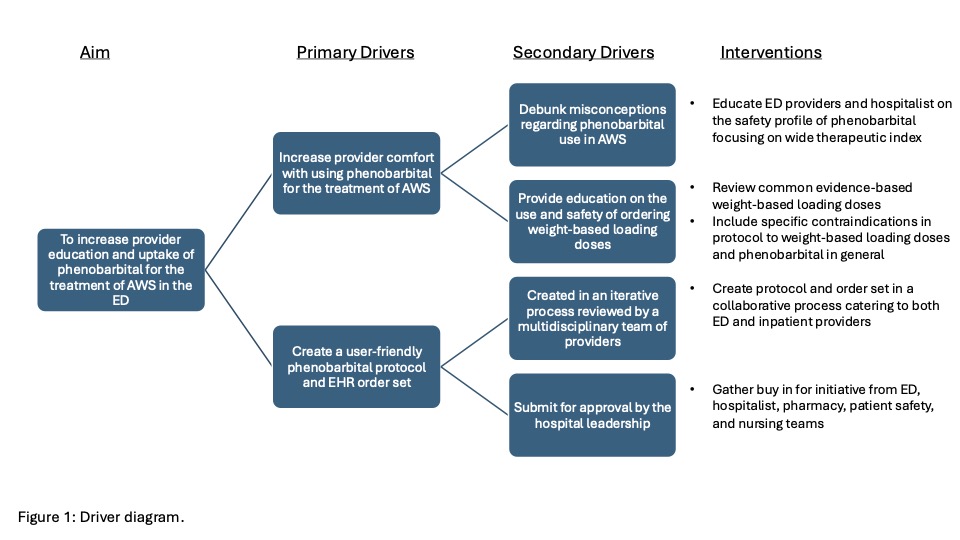
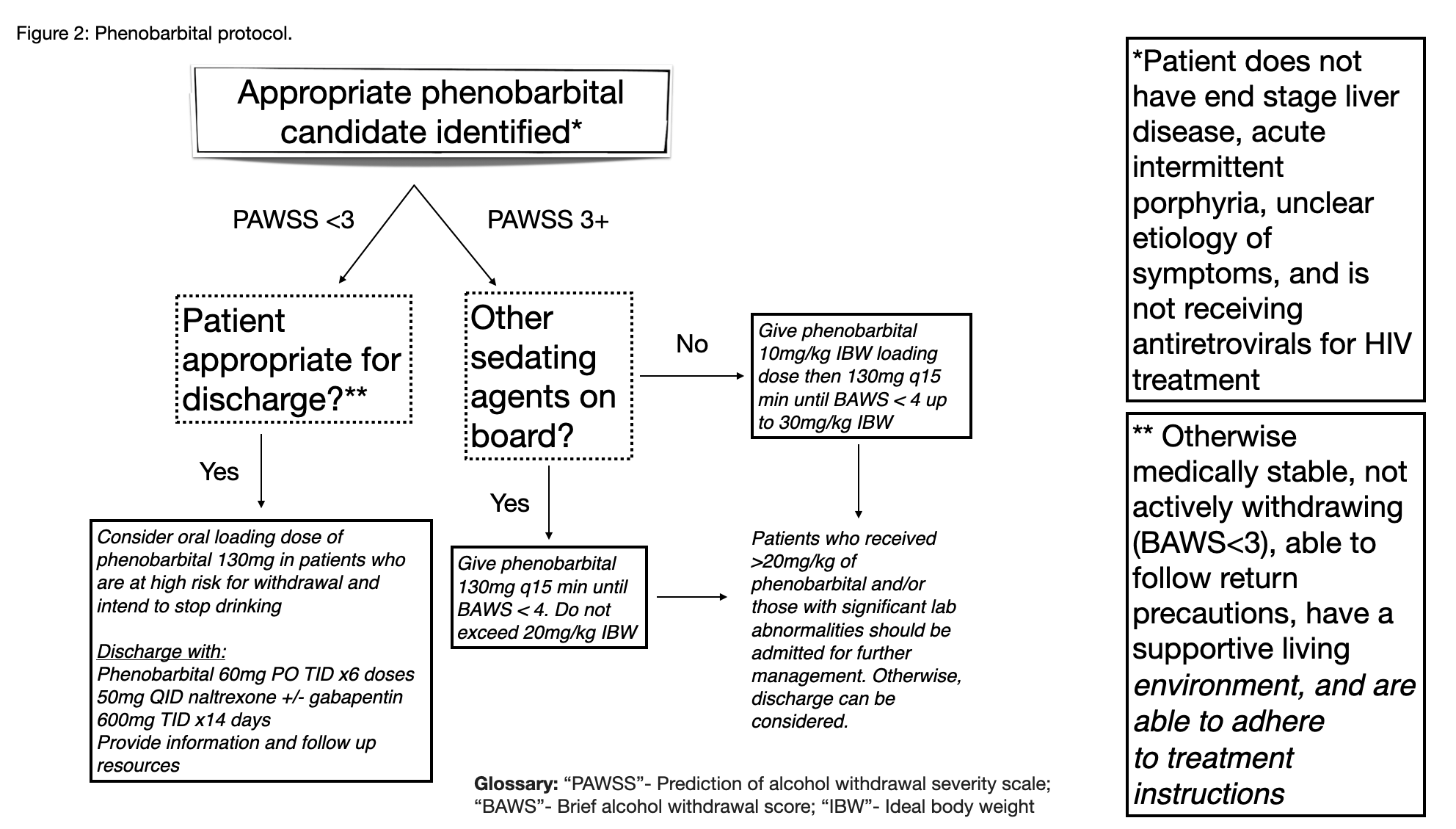
Description: Mountain West Medical Center (MWMC) is a rural affiliate hospital of the University of Utah hospitals (UUHC). In 2020, the UUHC academic hospitalist group entered an innovative partnership with MWMC and took over inpatient care with the goal of improving its quality of care and promoting evidence-based medicine.InterventionOur intervention was multifaceted and included: 1) Identification of key ED and Hospitalist stakeholders to form a working group. 2) Review of all AWS protocols from both institutions. 3) Gathering input from providers on experience in using phenobarbital for AWS. 4) Creation of a new phenobarbital protocol and electronic health record (EHR) order set. 5) Monthly PDSA cycles to seek feedback, understand barriers, change processes, and promote education (figure 1). Provider education and perspectivesMost hospitalist had limited experience using phenobarbital for AWS. Some described using it initially during the COVID-19 pandemic when rates of severe AWS rose, but ICU beds were full. Despite familiarity, many hospitalists did not feel comfortable with the high loading doses required to effectively treat AWS given concerns already mentioned. While many ED providers were familiar and comfortable with its use, many were hesitant to administer it as they thought that the admitting hospitalist may not feel comfortable accepting patients that received the medication. We thus held educational sessions for both groups of providers reviewing the data and safety profile of phenobarbital for AWS.Creating a phenobarbital protocol A protocol was created in collaboration with the ED, hospitalist, pharmacy, and nursing teams (figure 2). The framework was based on existing protocols at other academic institutions including UUHC and provided guidance regarding weight-based loading doses.
Conclusions: Implementing new evidence-based treatment protocols pioneered at AMCs can be difficult in any health care setting but is particularly pronounced in rural hospitals [9]. While lack of provider familiarity was a significant barrier, our implementation process also highlighted the importance of communication between the various hospital stakeholders.