Background: Hospitalized patients may require central venous access devices (CVADs) for inadequate intravenous (IV) access. CVADs have known complications, including peri-procedural trauma and central line associated bloodstream infections (CLABSI). CLABSI is of concern for patients and hospital systems, as it is largely preventable and used as a quality measure. A CVAD alternative is a short IV catheter inserted into an internal jugular vein, called a “peripheral IJ” (PIJ). PIJ catheters eliminate the need for tissue dilation during placement, are not considered CVADs, and are less likely to cause pneumothorax or significant arterial damage due to their shorter length and smaller gauge. We describe the implementation and outcomes of a pilot study for PIJ placement by a medicine procedure service (MPS).
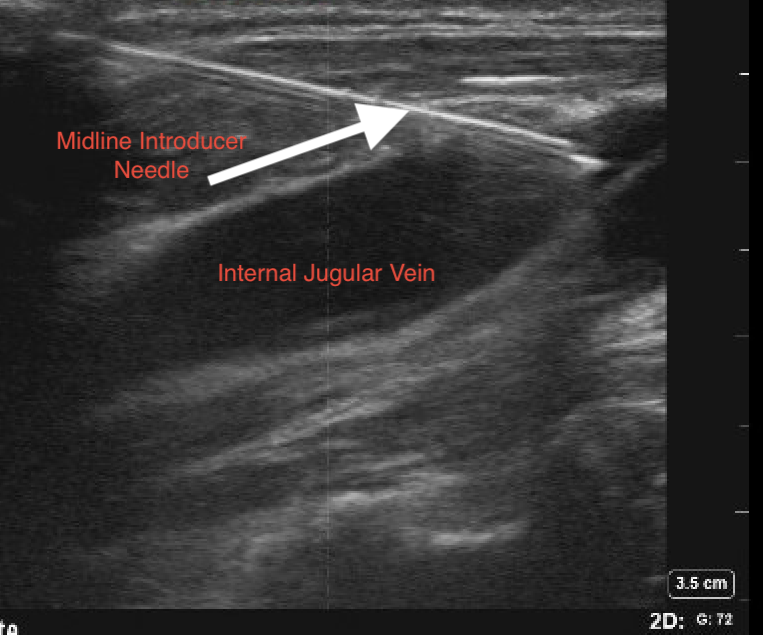
Methods: In December 2020, we sent all MPS faculty a survey of PIJ device familiarity, followed by an educational video describing best practice for PIJ insertion, further reinforced by discussion at a faculty meeting in March 2021. Faculty then had discretion after consultation for inadequate venous access whether to place PIJ instead of a CVAD. Appropriate candidates were patients needing short term venous access and not receiving medications requiring central access. Faculty used 10 cm, 14-French midline catheters, 6 cm wire introducer angiocaths, or 4.5-6.5 cm peripheral IV catheters depending on availability and preference. All devices were placed under real-time ultrasound guidance (Figure 1). Outcomes included duration of use, catheter failure (defined as catheter occlusion or migration), and whether the patient subsequently needed a non-tunneled CVAD during that encounter. We did not measure subsequent tunneled or peripherally inserted central catheters as these were felt to be separately indicated. We also evaluated differences in outcomes for midline vs. other catheter placements, with statistical significance measured with t test for continuous and Fisher’s exact test for categorical variables.
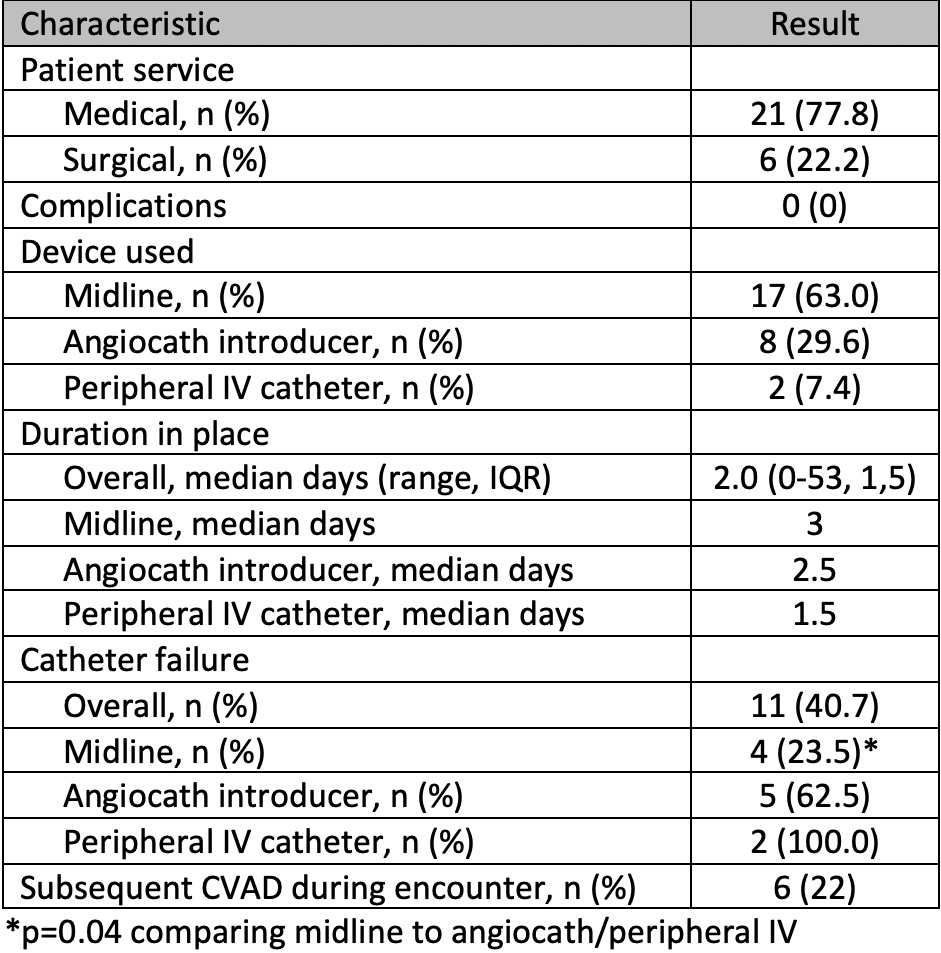
Results: Between March 2021 and November 2022, we attempted 28 PIJ catheter placements. Of these, 27 (96.4%) were successfully placed in 25 patients (two patients had two PIJs in separate encounters). Mean patient age was 53 years, and 80% were women. Characteristics of the 27 placed PIJs are displayed in Table 1. The majority were in medical patients and there were no procedural complications. Median duration of use was 2.0 days (range 0-53, IQR 1,5). While 11/27 (40.3%) of catheters eventually failed, midlines were much less likely to be removed due to failure compared with angiocath introducers and peripheral IVs (23.5% vs. 70.0%, p=0.04). A minority of patients, 6 (22%) patients needed subsequent non-tunneled CVAD during the encounter.
Conclusions: The large majority of attempts at PIJ placement for inadequate venous access by a MPS were successful and had no complications. While median duration of use was short, less than one-quarter of patients required subsequent placement of a non-tunneled catheter during the encounter. Comparing catheter types, midlines were significantly less likely to be removed due to failure. Our results suggest that health care systems can consider PIJs as a means to avoid CVADs and their associated procedural and CLABSI risks in select patients