Background: The Michigan PICC-DVT Risk Score (MRS) identified five predictors for deep venous thrombosis (DVT) associated with peripherally inserted central catheters (PICCs): presence of another central venous catheter (CVC) when device is placed, white blood cell (WBC) count at time of insertion, active cancer, number of catheter lumens, and history of venous thromboembolism (VTE)1. We sought to determine if these risk factors can also predict DVT in patients receiving midline catheters (midlines), which are shorter peripherally inserted devices associated with a similar risk of DVT as PICCs.
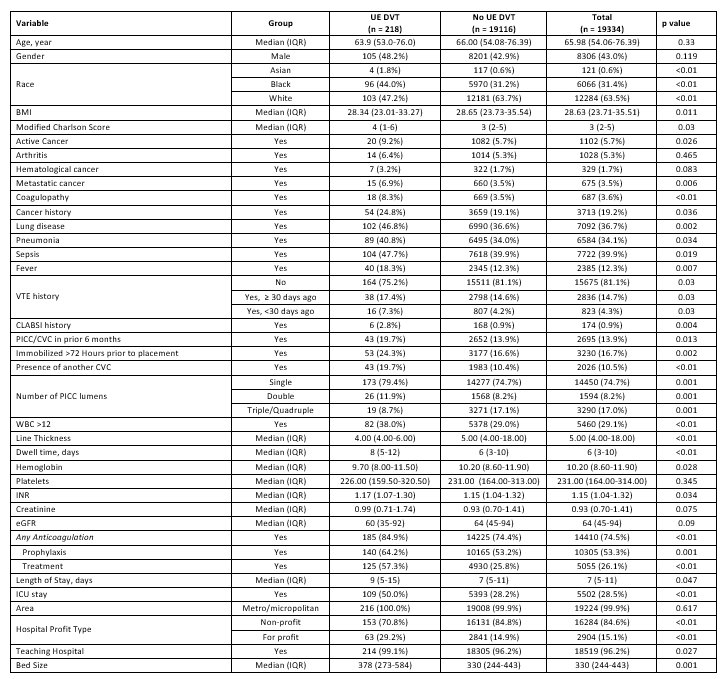
Methods: From December 2016 to July 2022, trained abstractors collected demographic and clinical data on patients receiving midlines while admitted at 64 hospitals participating in the Michigan Hospital Medicine Safety Consortium, a collaborative quality initiative funded by Blue Cross Blue Shield of Michigan. Patients were followed until midline removal, death, or 30 days post device insertion, whichever came first. The primary outcome was image-confirmed symptomatic upper-extremity DVT. Patient and device characteristics of midline placements with an upper-extremity DVT were compared to those without a DVT. All comparisons used Chi-square tests for categorical variables and t-tests and Wilcoxon rank-sum tests for continuous variables. We evaluated the association between MRS predictors and DVT in midline recipients using a mixed-effects logistic regression model which accounted for hospital-level clustering. Model discrimination was assessed through area under the curve (AUC) receiver operating characteristic analysis.
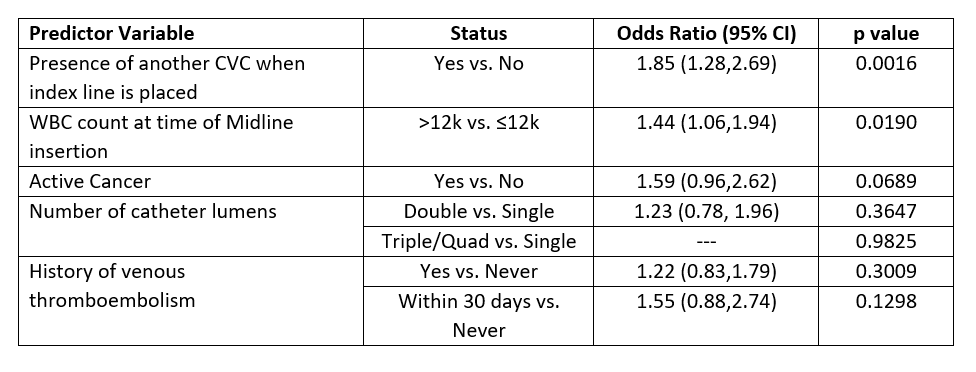
Results: A total of 19,334 midlines were included. The rate of upper-extremity DVT was low and occurred in 218 (1.13%). All MRS predictors were more common in midlines with a DVT than those without: presence of another CVC (19.7% vs. 10.4%; p< 0.01), an elevated WBC count (38.0% vs. 29.0%; p< 0.01), active cancer (9.2% vs. 5.7%; p=0.026), a double-lumen midline (11.9% vs. 8.2%; p< 0.01), and a history of DVT (24.8% vs. 18.9%; p< 0.01). However, after multivariable adjustment and accounting for hospital-level clustering, only two of the five MRS predictors for PICC-DVT were also found to be predictive of DVT in midlines: presence of another CVC (odds ratio [OR] 1.85; 95% CI: 1.28-2.69) and WBC >12 k/microliter at time of insertion (OR 1.44; 95% CI: 1.06-1.94). Model calibration was driven by hospital-level variation more than predictor variables. The AUC was 0.732 when the predicted probability of an event included the random-effects for hospitals, but only 0.599 when hospital-level effects were removed.
Conclusions: The Michigan PICC-DVT Risk Score provides low predictive power for midline-associated DVT. Based on the low rate of midline-associated DVT in our sample, the poor predictive power could be a result of the infrequent outcome, or it could be an indication of other patient and device characteristics driving DVT events in the midline population. A larger sample size may be necessary to develop an independent risk score for determining predictors of midline- associated DVT.