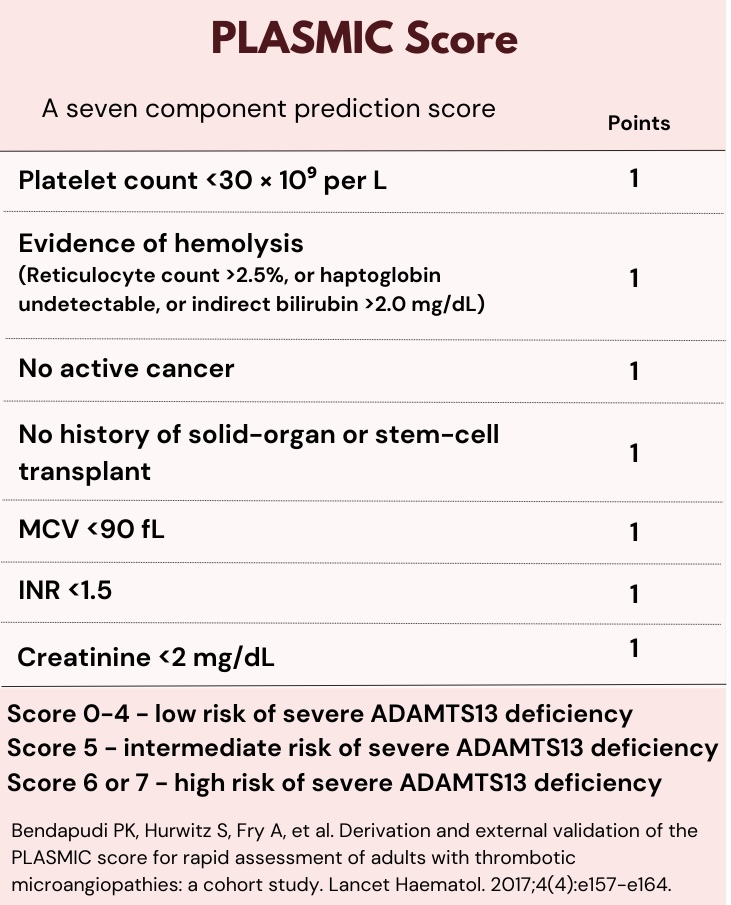
Case Presentation: A 19-year-old woman presented to an outside hospital with 2-hours of slurred speech and right-sided paresthesia. Her past medical history was significant for obesity and gastric sleeve surgery. Vitals showed blood pressure of 156/98 mmHg, pulse of 96 bpm, respiratory rate of 18 bpm, and oxygen saturation of 100% on room air. The neurological exam was normal, and symptoms resolved while waiting for evaluation. Labs showed hemoglobin 8.5 g/dL, MCV 89 fL, platelets 42 K/cumm, creatinine 1.07 mg/dL, total bilirubin 2.9 mg/dL. CT head was unremarkable. The anemia was attributed to hypermenorrhea and the neurological symptoms to stress related conversion reaction. She was discharged home with iron supplementation. Four weeks later, she presented with a recurrent episode of right-sided paresthesia and slurred speech. She also had a frontal headache, nausea, and abdominal pain. She denied any diarrhea, fever, or recent antibiotic use. Work up showed hemoglobin 6.2 g/dL, platelets 9K/cumm, creatinine 4.1mg/dL, total bilirubin 8.2mg/dL, lactate dehydrogenase 1342 units/L, haptoglobin < 30 mg/dL, C3 95 mg/dL, C4 5.9 mg/dL, negative HIV, hepatitis B, and hepatitis C. Autoimmune testing with rheumatoid factor, antinuclear antibody (ANA), extractable nuclear antigen (ENA), anti-cyclic citrullinated protein antibody (anti-CCP), antineutrophil cytoplasmic antibodies (ANCA), antibodies against glomerular basement membrane (anti-GBM), and antiphospholipid antibody panel were negative. Urine drug screen was negative, and blood cultures and urinary cultures had no growth. Peripheral blood smear showed schistocytes. Repeat CT head was negative for acute findings. Brain MRI with and without contrast was concerning for focal infarcts. The suspected diagnosis was Thrombotic Thrombocytopenia Purpura (TTP). The PLASMIC score was 6 (high risk). The patient underwent plasmapheresis and received pulse dose steroids and rituximab. ADAMTS13 activity resulted in less than 5%, and ADAMTS13 inhibitor was elevated. She then received one dose of caplacizumab and had gradual improvement of symptoms.
Discussion: Thrombotic thrombocytopenic purpura is a rare thrombotic microangiopathy with high mortality rates caused by acquired or congenital deficiency of ADAMTS13, the Von Willebrand factor regulatory enzyme (1). Early diagnosis with urgent start of plasmapheresis is essential to decrease mortality. The PLASMIC score was validated in patients suspected of having a thrombotic microangiopathy to stratify the risk of severe ADAMTS13 deficiency and assist in the decision to start early treatment (2). Her PLASMIC score on initial presentation was 5 (intermediate risk) which would have warranted further work up. This case is relevant to hospitalists as it illustrates the importance of early recognition of TTP in patients presenting with neurological symptoms, thrombosis, acute kidney injury, thrombocytopenia, and hemolysis.
Conclusions: Common symptoms such as anemia can often be overlooked. We present this case to enforce the importance of attention to other red flags when framing clinical presentations to avoid diagnostic bias. Early recognition and diagnosis of rare presentations such as TTP can be challenging, delaying treatment, and increasing morbimortality.