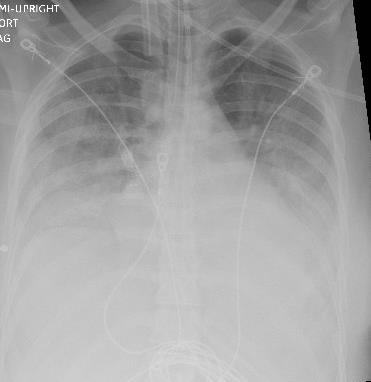
Case Presentation: A 26-year-old woman presented following accidental ingestion and aspiration of lighter fluid during a fire-breathing performance. She noted difficulty breathing, significant oral pain, and a burning sensation in her throat and chest.Initial vitals were notable for tachycardia to 110s, tachypnea to mid-20s, and oxygen saturation of 100% on non-rebreather mask. She appeared anxious and in distress, coughing continuously and inhaling with difficulty. Physical examination revealed lungs clear to auscultation and no visible burns in the oropharynx. She was intubated given concern for impending airway compromise.Serial chest x-rays showed increasing confluence of bilateral midlung-basal opacities and pleural effusions suggestive of evolving acute lung injury and pneumonitis. Bronchoscopy revealed significant inflammation, friability, and patchy erythematous mucosa with some edema. Secretions were minimal and clear without any evidence of soot, burn injuries, or active areas of bleeding. Initial ABG demonstrated pH 7.31, pO2 77 mm Hg, pCO2 45 mm Hg, FiO2 40%, and HCO3 22 mEq/L. Her PaO2/FiO2 ratio worsened to 89, consistent with severe acute respiratory distress syndrome (ARDS).The patient required vasopressors and ventilatory support. Given her developing fever and leukocytosis, she was treated with vancomycin, piperacillin/tazobactam, and azithromycin for suspected superimposed aspiration pneumonia. All subsequent infectious work-up was negative. She completed a 7-day course of steroids given the severity of her pneumonitis. She was also administered intravenous proton pump inhibitor and diuresis as supportive measures. After 7 days, she was extubated, slowly weaned off oxygen, and discharged home.
Discussion: Lighter fluids are aliphatic hydrocarbons, which when aspirated, can cause multi-organ toxicity. The most clinically significant side effect is pulmonary toxicity (lipoid pneumonia) via dissolution of surfactant and necrosis of pulmonary tissue. Patients’ symptoms develop rapidly within 24 hours, progressing to respiratory failure and ARDS. Secondary infection, suggested by persistent fever, can exacerbate the initial aspiration pneumonitis. Other hydrocarbons that may induce similar pulmonary symptoms include several household and industrial products (e.g. paint thinners, lotions, and cleaning agents), which have addictive potential given their euphorigenic character. While generally associated with hydrocarbon aspiration, the diagnosis of lipoid pneumonia assumes even more clinical significance given the recent prevalence of e-cigarette, or vaping, product use-associated lung injury (EVALI). A differential diagnosis of lipoid pneumonia among these patients has been considered based on history of using liquids in e-cigarettes which contain sources of lipid, consistent radiologic findings, and demonstration of lipid laden macrophages in respiratory samples.
Conclusions: Fire-breather’s pneumonia is a severe chemical pneumonitis resulting from aspiration or inhalation of hydrocarbons. It is a rare but life-threatening condition among fire performers. Secondary complications include ARDS and bacterial superinfections. Symptoms of respiratory distress after hydrocarbon ingestion should prompt early supportive intervention to minimize risk of progression to ARDS.