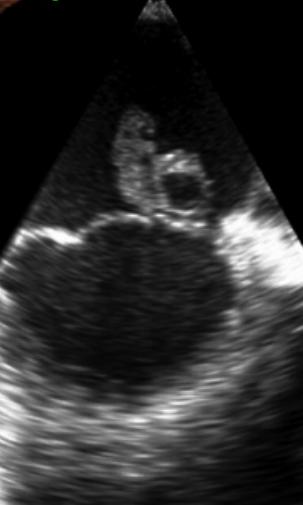
Case Presentation: A 30 year-old female presented postpartum day 1 following a normal vaginal delivery from an outside hospital after chest CT angiography (CTA) identified a 2.5 cm pericardial effusion. Review of systems was positive for dry cough, left sided chest pain, dyspnea on exertion, recent post-partum abdominal pain, chills, and diaphoresis. On arrival to the medicine floor, she was afebrile, BP: 140/83 without pulsus paradoxus, HR 100 bpm, RR 20, and normal O2 saturation on room air. Physical exam revealed rales at the lung bases, bilateral pedal edema, and JVD to angle of the mandible. Labs were significant for a WBC 22,700, procalcitonin of 1.78, ESR 52, CRP 128, BNP of 587, and troponin peak of 0.110. EKG showed no ST changes and was without electrical alternans. On initial evaluation, a bedside Point of Care Ultrasound (POCUS) exam of the heart was performed, which was concerning for ~2 cm vegetation on the mitral valve (POCUS Mitral Vegetation Image). As a result, the patient was immediately started on empiric vancomycin and piperacillin-tazobactam due to concern for sepsis from infective endocarditis (IE). A formal TTE performed the following morning confirmed a vegetative mass measuring 2.2 cm x 1.5 cm on the anterior leaflet of the mitral valve with mitral regurgitation, dilated left atrium, and pericardial effusion. TEE further confirmed the presence of a large vegetative mass with multiple echolucencies suggestive of valvular abscess (TEE Mitral Vegetation Image) . Blood cultures came back positive for Streptococcus mitis/oralis . Cardiothoracic Surgery was consulted and performed an immediate mitral valve repair with abscess extraction. She was discharged home with 6 weeks of IV ceftriaxone and follow up with Infectious Disease. It is important to note, the baby was also tested and luckily the blood cultures remained negative at > 5 days.
Discussion: The utility of POCUS in evaluating cardiovascular disease has been evaluated at length in inpatient and outpatient settings. In the inpatient setting, POCUS exams can evaluate and help manage conditions such as shock, cardiac arrest, acute heart failure and valvular pathology. However, the ability to evaluate for these conditions remains primarily dependent on the hours of training received (Kovell, 2018; Luong, 2018) and the formal programs designed for trainees. According to the American Heart Association guidelines, a TEE is the recommended initial test in high-risk individuals with suspected IE. This is due to low sensitivity of TTEs in detecting vegetation in comparison (Biswas and Yassin, 2015). However, a quick POCUS exam as above can be an invaluable tool when a formal TTE or TEE is not readily available.
Conclusions: This case exemplifies how cardiac POCUS expedited a preliminary diagnosis and directly influenced early initiation of antibiotics. POCUS is an invaluable tool to manage cardiovascular conditions as above, and its utility extends beyond the cardiovascular system. However, the ability to assess for certain conditions with POCUS is directly related to the extent of each individual’s training. As such, formal POCUS training by means of a “Teach the Teacher” model has been implemented at Wake Forest Baptist Medical Center, which has led to an overall improvement in comfort and bedside skill using this technology. We argue that all hospitalists should be trained in bedside ultrasound, and POCUS should be considered as an extension of the physical exam to further evaluate certain medical scenarios in the acute inpatient setting.
.jpg)