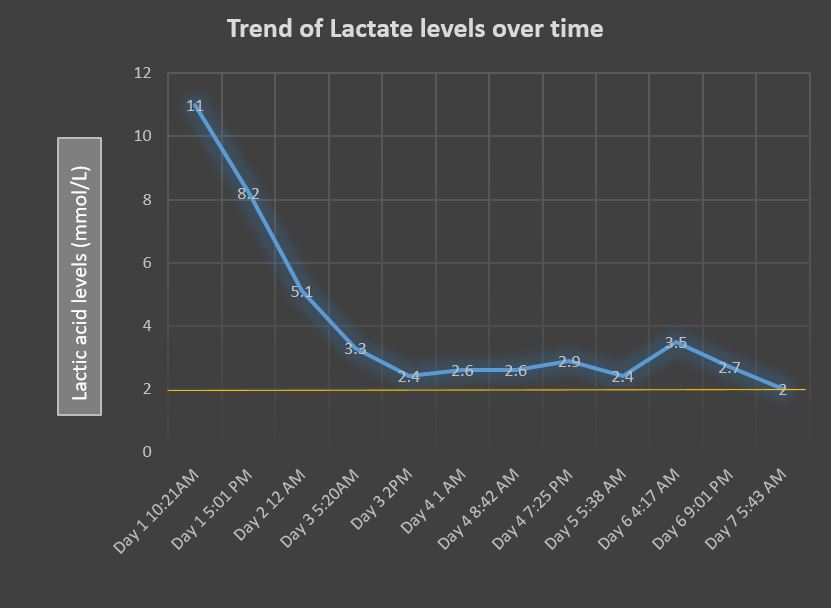
Case Presentation: 85-year-old woman with a past medical history of hypertension, severe peripheral vascular disease, atrial fibrillation on Coumadin was hospitalized to have lower extremity above knee amputation for long standing infection of the left lower extremity. Patient was started on cefepime and linezolid for her left lower extremity wound (cultures growing pseudomonas, vancomycin resistant enterococci and methicillin resistant staphylococcus aureus). As part of preoperative clearance, she underwent an echocardiogram which revealed severe aortic stenosis for which she underwent a balloon valvuloplasty. On day 5 of Linezolid, patient became hypotensive and confused on the medical floors necessitating transfer to the intensive care unit. Her labs revealed a high anion gap metabolic acidosis (bicarbonate of 15 mEq/L, anion gap of 19 mEq/L) which lead the provider to check lactate levels. Lactic acid levels were noted to be 11 mmol/L. She was managed with intravenous fluids and bicarbonate infusion. Linezolid induced lactic acidosis was suspected and antibiotics were changed to meropenem and daptomycin. Patient also developed thrombocytopenia later in the hospitalization, attributed to linezolid toxicity. Lactate levels were followed and took seven days to normalize. Patient’s mental status improved, she medically stabilized and successfully underwent an above knee amputation of the culprit limb after her acidosis improved.
Discussion: Linezolid is an oxazolidinone antibiotic which is increasingly important in this age of antibiotic resistance. It is used to treat drug resistant, gram positive bacterial infections such as Vancomycin resistant enterococci (VRE) and Multidrug Resistant Staphylococcus Aureus (MRSA). It is essential for physicians to be aware of the life threatening complications of this commonplace antibiotic- namely lactic acidosis induced by linezolid.Linezolid acts by inhibiting bacterial protein synthesis by binding to bacterial ribosomes. Because of the similarity between bacterial ribosomes and mitochondrial ribosomes, linezolid can cause mitochondrial toxicity inhibiting mitochondrial protein synthesis and leading to lactate accumulation. Organ systems that are highly dependent on oxidative metabolism include the brain, kidneys, retina and skeletal muscles- these are generally involved in mitochondrial toxicity. Lactic acidosis induced by linezolid is a life threatening complication with a high mortality rate of nearly 25%. This is generally seen in the 6th week of treatment although there have been reports of lactic acidosis occurring after a much shorter treatment duration, such as the case described here. Symptoms such as nausea, vomiting, altered mental status and supporting laboratory findings of metabolic acidosis, elevated anion gap, thrombocytopenia and hypoglycemia should raise suspicion of linezolid induced lactic acidosis. A high degree of suspicion is necessary, as discontinuing linezolid is the mainstay of treatment. Patients may sometimes need hemodialysis to help them clear the drug and intravenous thiamine which is a co-factor of respiratory chain enzymes. Lactic acid levels can sometimes take up to 15 days to clear.
Conclusions: This case highlights that physicians should be aware of this dangerous complication of linezolid use which requires prompt cessation of linezolid and aggressive medical support.