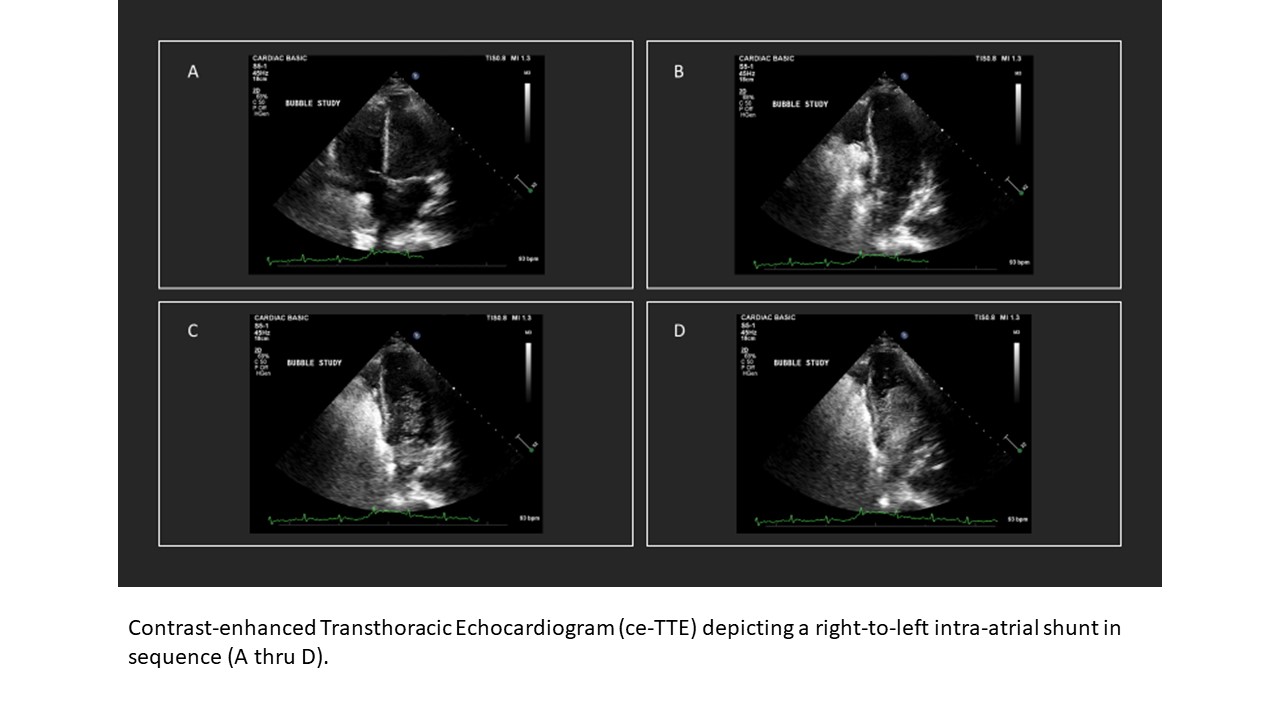
Case Presentation: The patient was a 28-year-old male with past medical history significant for polysubstance abuse including alcohol and opiates, as well as chronic DVTs on coumadin, who originally presented to the hospital for recurrent pancreatitis. Two weeks into his admission, he abruptly became hypotensive (MAP < 65mmHg), tachycardic, and hypoxemic (SpO2 < 88% on room air). The patient was placed on a non-rebreather mask and an ABG showed a pH of 7.47, pCO2 of 25, and a pO2 of 68. His INR at the time was 6.6 (supratherapeutic with goal of 2-3). A rapid physical exam showed the patient’s left lower extremity to have 1+ non-pitting edema with none appreciated on the right, however this was unchanged since admission. Auscultation of his lungs found bibasilar rhonchi, with no wheezing or rales. An EKG showed sinus tachycardia with a heart rate of 150. BNP-pro and Troponin labs were obtained, and both were elevated at 6,142pg/mL (ULN < 125) and 0.084ng/mL (ULN < 0.035). Given concern for the development of an acute, massive PE, a stat CT angiogram of his thorax was obtained which demonstrated no pulmonary embolism but did find small bilateral pleural effusions with adjacent consolidative opacities and diffuse ground glass centrilobular nodules concerning for multifocal pneumonia vs. ARDS. Given these findings, the patient was started on antibiotics and upgraded to the ICU for further evaluation and treatment.While in the ICU, the patient quickly stabilized and was rapidly weaned back down to nasal cannula at 2lpm. Despite this, over the next four days, the patient had multiple episodes of the same clinical scenario; tachycardia, hypoxemia, and hypotension. Due to concern for a shunt (either intrapulmonary vs intracardiac), a contrast-enhanced echocardiogram (ce-TTE) was obtained which demonstrated a right-to-left atrial shunt (patent foramen ovale or PFO) with dilated right atrium and mildly elevated estimated pulmonary artery pressure (PAP) (Figure 1). The patient ultimately improved with treatment of his pneumonia and is undergoing an ongoing workup for potential closure of his PFO.
Discussion: Hypoxemia has a broad differential, and timely diagnosis and management is critical. In patients with tachycardia and hypoxemia, PE should be considered, but not exclusively. Hemodynamic sequelae of intra-atrial shunts, including PFOs, are poorly understood. Among other consequences including paradoxical emboli, episodic hypoxemia is a known issue (1, 2, 3). Conditions that cause increased PAP, such as mechanical ventilation, may worsen shunting and the associated symptoms (4). Diagnosis with ce-TTE is currently the gold standard and may also show right-heart dilation and elevated pulmonary pressures.
Conclusions: – PE must remain high on the differential for any patient with tachycardia and hypoxemia- Intra-cardiac shunting should be considered in episodic hypoxemia events, and is best evaluated with a ce-TTE- Events such as PE or pneumonia that increase pulmonary arterial pressure, may cause an intracardiac shunt to present or worsen