Background: Children with medical complexity (CMC) are a growing pediatric population with disproportionately high health needs and costs often insured by Medicaid. Identification of CMC using complexity classification systems applied to population-level data and establishment of baseline patterns of population-level health care utilization are essential to target patients who may benefit most from complex care management. Despite the potential applications, the CMC population has yet to be systematically identified within the Medicaid pediatric population statewide in North Carolina (NC), and their unique patterns of healthcare utilization have not been established.
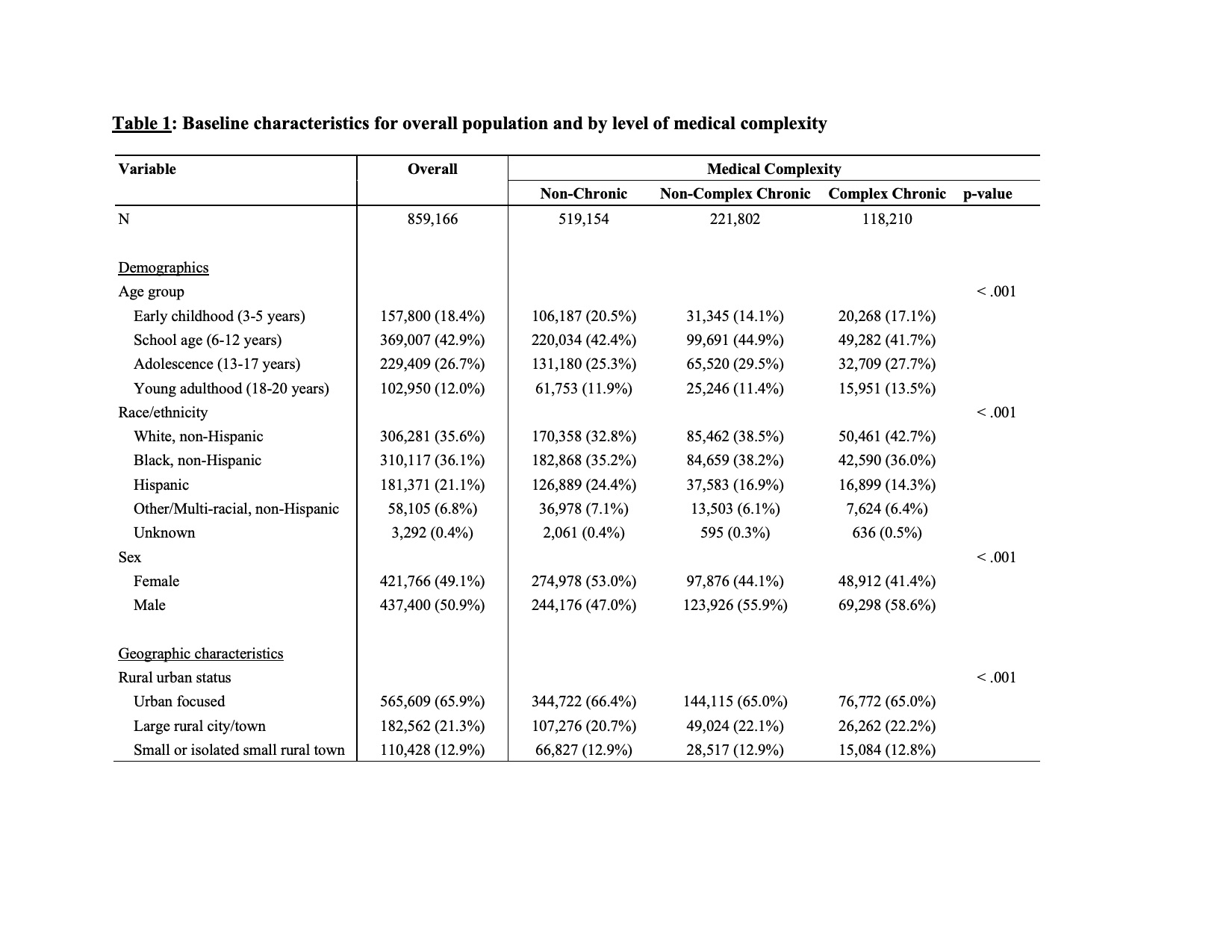
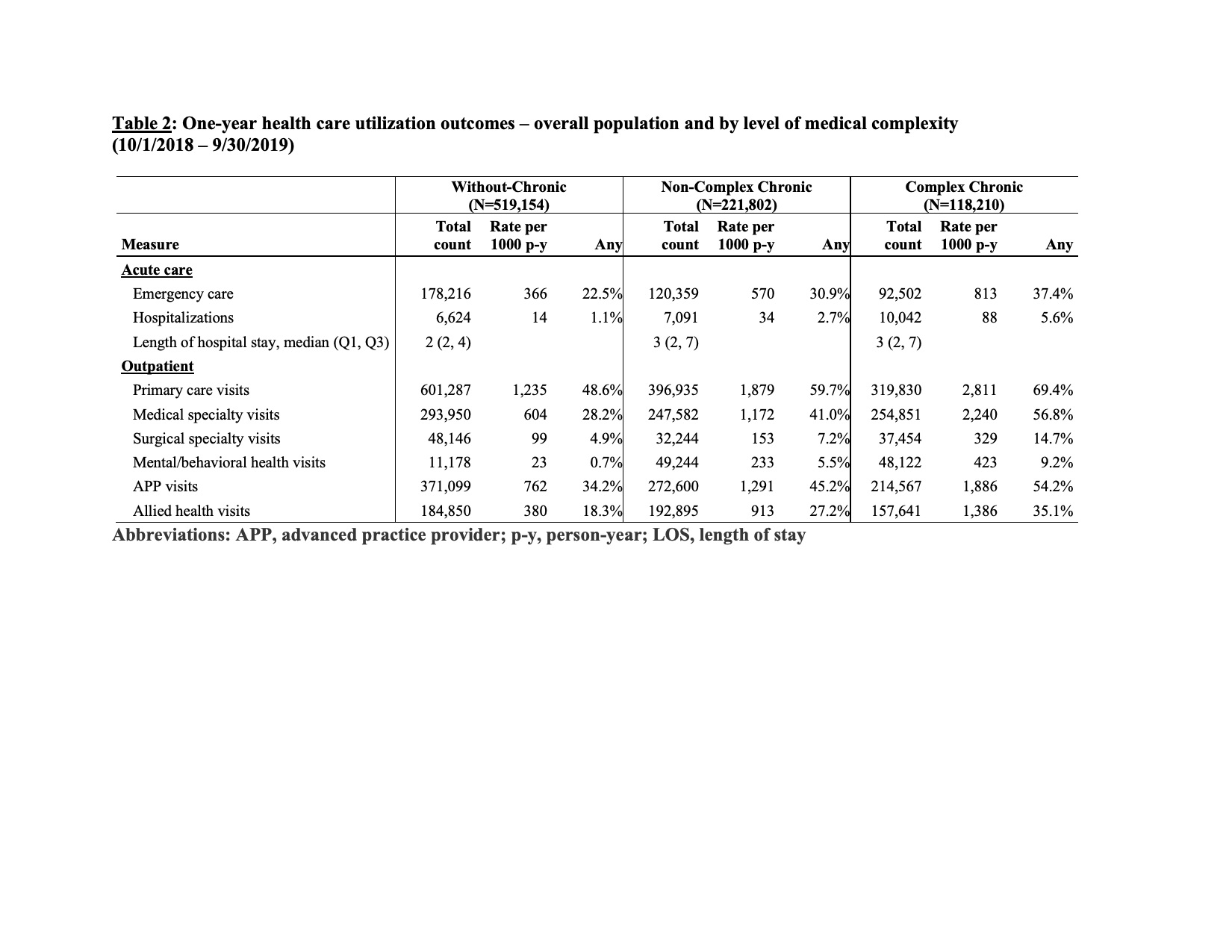
Methods: The study objectives were to: (1) characterize health care utilization and costs for a statewide population of Medicaid-insured children by medical complexity level and (2) to assess differences in health care utilization for CMC by race/ethnicity and rurality. This was a retrospective, secondary analysis of NC Medicaid administrative claims between 10/1/2015 –9/30/2019 for 859,166 enrollees ≤20 years old with three years continuous Medicaid enrollment. We applied the validated Pediatric Medical Complexity Algorithm (PMCA) to classify children into three complexity groups: without chronic disease (W-CD); non-complex chronic disease (NC-CD); and complex chronic disease (C-CD). Medical complexity level was defined on 9/30/2018; health care utilization and costs were summarized for the subsequent one-year period (10/1/2018 – 9/30/2019). Utilization rates (per 1,000 person-years) were calculated per group. Health care utilization and costs included acute (hospitalization, ED/urgent care) and outpatient care (primary, specialty, allied health, pharmacy). Costs were summed per-person and reported as median (Q1, Q3) and proportion with any cost over one year. Race/ethnicity and rural-urban classification of home residence were identified in NC Medicaid claims; race/ethnicity and rurality were compared within complexity groups using rate ratios adjusted for age.
Results: Among 859,166 NC Medicaid-insured children, 60% were W-CD, 25.9% were NC-CD, and 13.8% were C-CD. Acute and outpatient care utilization, and annual per-child costs were highest for children with C-CD [median (IQR) for C-CD=$1,913 ($572-$4,878) vs NC-CD=$884 (237-2,432) vs W-CD=$269 (21-779)]. Black, non-Hispanic children with C-CD experienced higher hospitalization (RR=1.12; 95% CI: 1.08–1.17) and lower outpatient visit rates compared to white, non-Hispanic children with C-CD; outpatient care utilization varied by visit type for children with C-CD living in rural settings compared to children with C-CD in urban settings.
Conclusions: Higher health care utilization and costs were associated with higher medical complexity for NC Medicaid-insured children. Healthcare utilization for children with C-CD varied significantly by race and rurality.