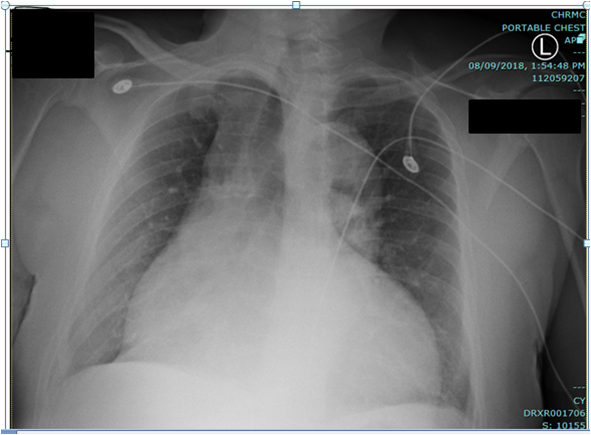
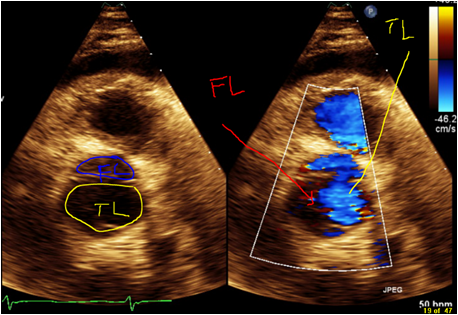
Case Presentation: A 57-year-old African-American male, with past medical history of nonischemic cardiomyopathy, moderate aortic insufficiency, HTN, and cocaine abuse presented to the emergency room with complaints of shortness of breath (SOB), and chest pain (CP). He admitted to using cocaine on his birthday party, which was 5 days ago. After using cocaine he started having freezing substernal CP which were 5/10 in intensity, intermittent, nonradiating and associated with feeling of SOB. The patient’s CP resolved with sublingual nitroglycerin. In the last 17 months patient had been admitted in hospital four times with complains of SOB and CP with the following chronologic diagnosis: HTN emergency, Atrial flutter, Acute HF exacerbation. Prior CT Chest with contrast did not show any AoD. Cardiac catheterization done in the last admission showed no significant coronary artery disease. Cocaine has been reported positive in all these admissions. On physical exam he had grade two systolic murmurs at base; mild crackles at lung base, no pedal edema or jugular vein distension. ECG showed no acute findings. Serial troponins three times were normal. Chest x-ray showed cardiomegaly with new wide mediastinum. Trans-thoracic echocardiography showed unchanged aortic regurgitation and Stanford type A AoD. CT chest confirmed AoD type A with dissection propagating to abdominal aorta. Patient immediately was transferred to a tertiary center. He underwent emergency repair of aortic dissection. Post surgery, he recovered well and was discharged after three days of hospital stay.
Discussion: Cocaine accounts for the greatest number of drug-related ED visits and the highest number of drug related deaths among its users. Crack cocaine is accountable for only 1.8% of AoD. The rapid onset of its action triggers an abrupt hemodynamic response resulting in AoD. Daniel et al reported CP as a presenting symptom in 82% of patients with cocaine related AoD. The key to making the diagnosis of this fatal disease depends on how familiar we are with the well described atypical presentation. Classical findings may not be present and we should think beyond classic textbook descriptions. Performing a detailed risk factor profile for AoD on every chest pain patient as well as decreasing our own threshold to obtain imaging studies can help in diagnosing this serious disease that may be hidden in old complains.
Conclusions: Aortic dissection (AoD), is an uncommon life threatening condition with an incidence range from 2.6–3.5 per 100,000 patients/year. AoD occurs due to increased aortic wall stress from hypertension (HTN) and, less commonly, to genetic predisposition, inflammatory conditions and cocaine. AoD can be rapidly fatal, in almost 40% of patients and death may be erroneously attributed to another cause. Since it remains a challenge to diagnose and treat it is very important to have a high index of suspicion for AoD in a patient with known history of cocaine abuse.