Background: Thirty-day readmission rates are increasingly used among hospitals as a quality of care indicator since research has shown that higher than expected readmission rates often lead to poor patient outcomes and high financial costs. Causes of readmission tend to be multifactorial and possibly variable dependent on systems. To investigate predictors of 30-day readmission rates, our study examined patients admitted to the EVMS Academic Team at Sentara Norfolk General Hospital (SNGH).
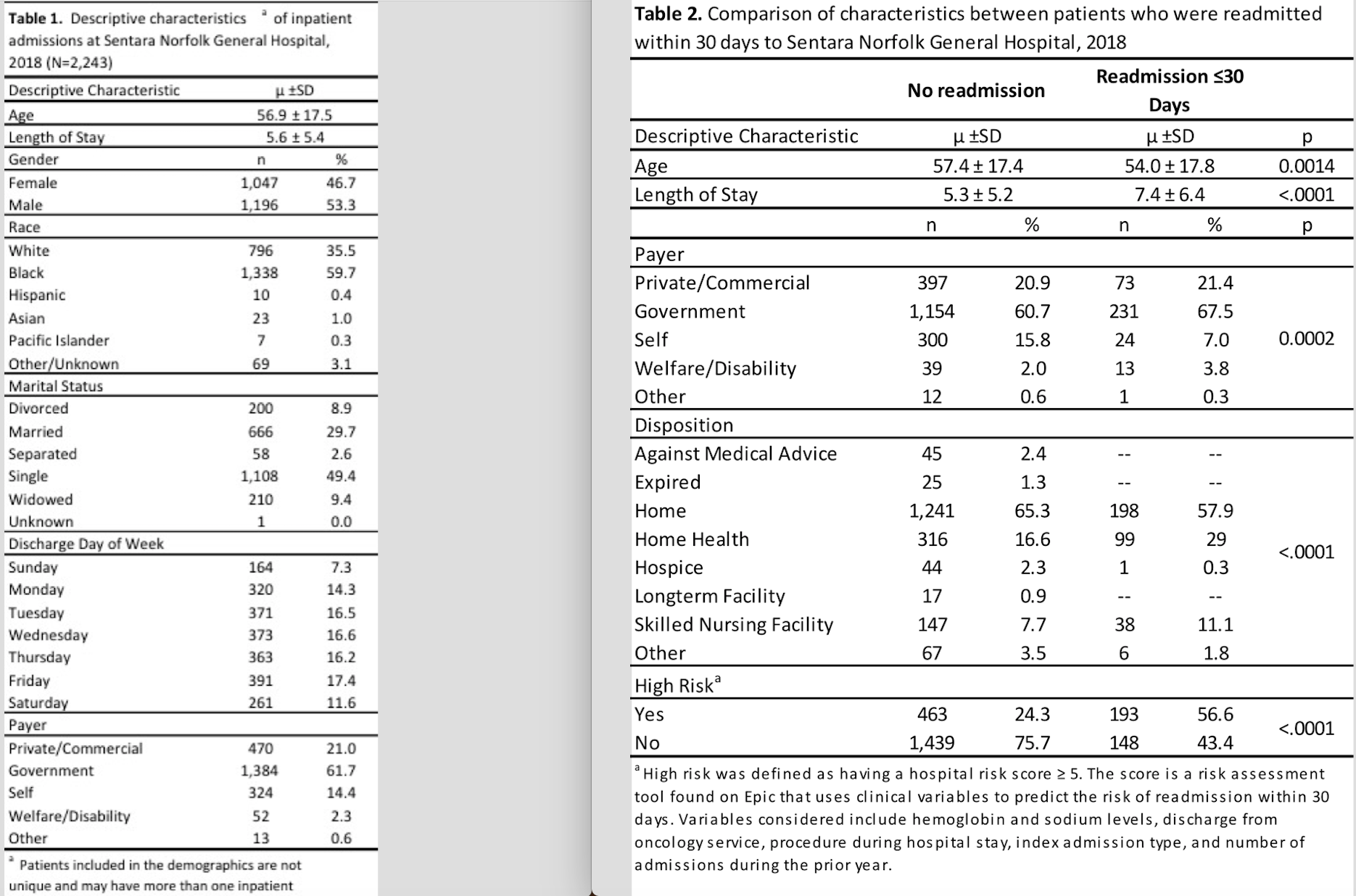
Methods: The study was conducted as a retrospective chart review of patients admitted to SNGH between January 1, 2018 and January 1, 2019. Patient records were reviewed for 14 parameters, including demographic, socioeconomic, and discharge factors. The data was analyzed using descriptive statistics and logistic regression.
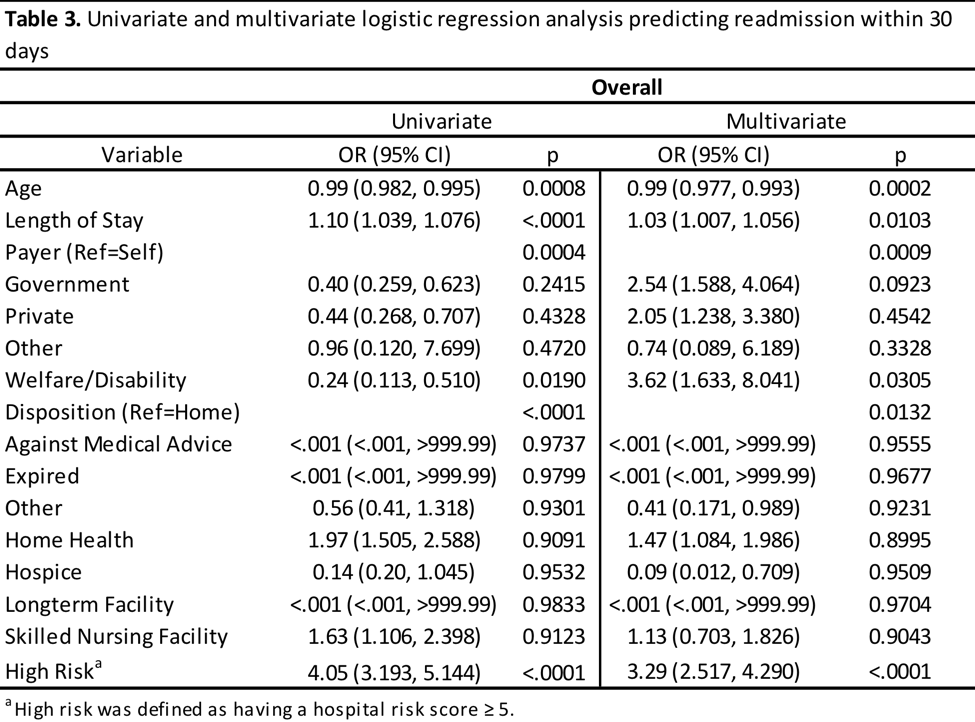
Results: There were 2,243 patients admitted to SNGH in 2018, 342 (15.2%) of which were readmitted. Demographic characteristics were similar between readmission groups and were not found to be independently associated with readmission. Age, length of stay (LOS), insurance payer status, disposition, and high-risk status (Hospital Risk Score ≥5) remained significant predictors of readmission in the multivariate regression model. The odds of readmission were 1.03 times higher for patients with a one day longer LOS (95% CI 1.007, 1.056, p=0.0103). Patients with government insurance were 2.54 (95% CI 1.588, 4.064) times more likely to be readmitted than those who paid out of pocket, while patients with private insurance were 2.05 (95% CI 1.238, 3.380) times more likely to be readmitted than out of pocket payers. Patients classified as high risk were 3.29 times more likely to be readmitted than those who were not (95% CI 2.517, 4.290, p<0.0001).
Conclusions: These findings will help SNGH identify patients who are at higher risk for readmission, with the hope of lowering readmission rates. While the significance of age, insurance, and LOS has been observed previously in the literature, the findings on disposition were unexpected and will require further investigation. These results also validate the use of the hospital risk score. Going forward, we intend to expand data collection to include readmissions to all hospitalist services at all Sentara hospitals over a five-year period.