Background: Inter-hospital transfer (IHT, the transfer of patients between hospitals) exposes patients to risks of discontinuity of care. To identify aspects of the transfer process that increase risk, we examined the impact of select transfer process factors on clinical outcomes among patients undergoing IHT.
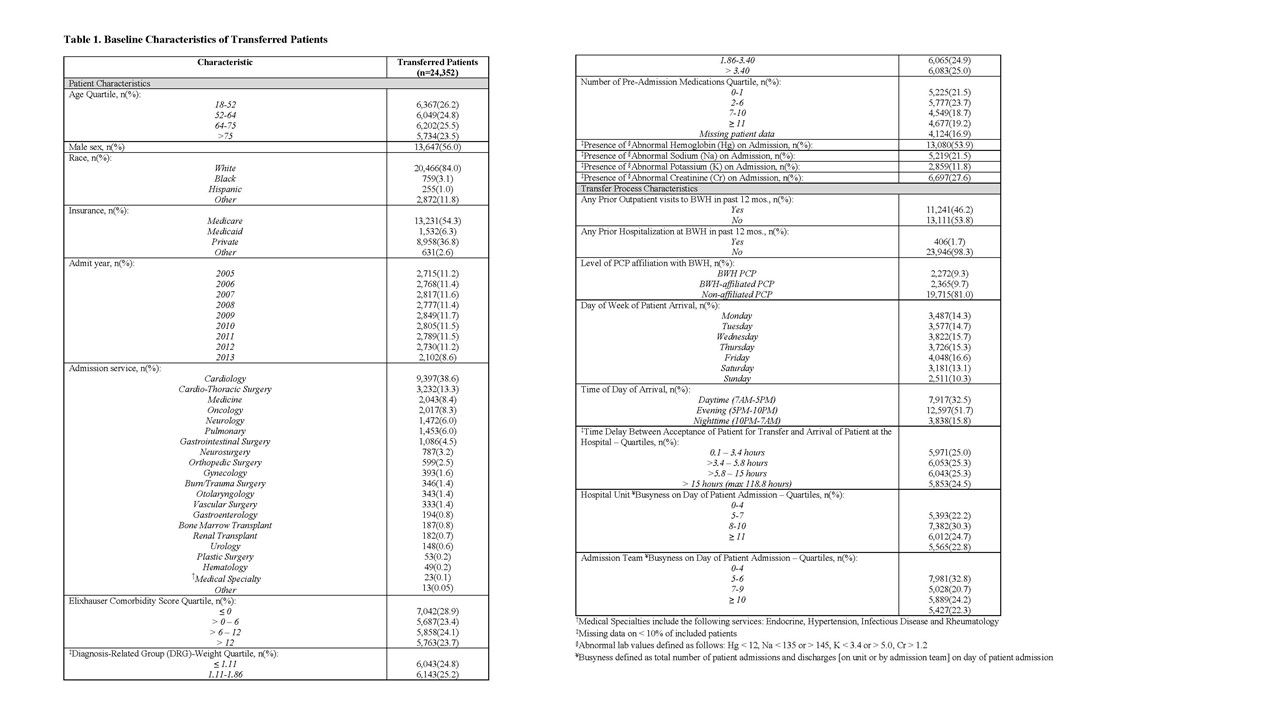
Methods: We performed a retrospective analysis of patients ≥ age 18 transferred to Brigham and Women’s Hospital (BWH), a 740-bed tertiary care hospital, from another acute care hospital between January, 2005 and September, 2013. Examined outcomes included transfer to the intensive care unit (ICU) within 48 hours of admission, and 3-day, in-hospital, and 30-day mortality from index admission. Potential predictors included any prior association with BWH (defined as prior outpatient visit, hospitalization or PCP affiliated with BWH), day of week of patient transfer, time of day of patient arrival, time delay between acceptance for transfer and arrival at BWH, and hospital unit and admission team busyness (admissions and discharges) on day of patient arrival. Covariates for adjustment included admission year and service, patient demographics, comorbidity, illness severity, number of preadmission medications, and selected abnormal laboratory values on admission. All data was obtained from administrative sources. We used descriptive statistics to determine baseline characteristics, and performed a series of multivariate logistic regression models to obtain the adjusted effect of each predictor on each outcome, adjusting for all other variables.
Results: 24,352 patients met our inclusion criteria (Table 1). We found that nighttime arrival (OR 1.65[95%CI 1.46,1.86]) and weekday arrival (OR 1.42[95%CI 1.31,1.54]) was associated with increased adjusted odds of ICU transfer, but time delay between acceptance and arrival, and hospital unit and admission team busyness on day of patient arrival were inversely associated with odds of ICU transfer and all mortality outcomes.
Conclusions: Our findings indicate that nighttime arrival increases risk of ICU transfer, potentially due to fewer overnight resources that may impact patient care decisions. We surprisingly found greater odds of ICU transfer in patients who arrived on a weekday, and greater odds of ICU transfer and mortality in patients with a short time delay, or those admitted to less busy hospital units or admission teams. These findings likely reflect confounding by indication, where sicker patients are transferred during the week and with less delay; and confounding by diagnosis (i.e. transfer to teams who care for sicker patients with less turnover). We plan to further study these outcomes stratified by service and patient diagnosis to better understand the impact of various processes of care on IHT outcomes.